Pharmaceutical Supply Chain: How Medications Get to You and What Can Go Wrong
When you pick up a prescription, you rarely think about the journey it took to get there. But the pharmaceutical supply chain, the complex network that moves drugs from manufacturers to patients. Also known as drug distribution system, it involves factories, wholesalers, distributors, pharmacies, and regulators—all working in sync just to get a pill into your hand. It’s not just about shipping boxes. It’s about ensuring the right drug, in the right dose, reaches the right person at the right time—without contamination, delays, or counterfeit products.
Behind every pill is a chain that starts with raw ingredients, often sourced overseas, then moves to labs where active ingredients are synthesized. From there, it goes to packaging facilities, then to regional distributors who handle bulk shipments. These distributors then send smaller batches to pharmacies, hospitals, and mail-order services. Any break in this chain—like a factory shutdown, a customs delay, or a shipping error—can cause drug shortages, when essential medications become unavailable. We’ve seen this with antibiotics, insulin, and even basic painkillers. And when shortages hit, doctors have to switch prescriptions, patients face delays, and some end up without treatment.
The rise of generic drugs, lower-cost versions of brand-name medications. has added another layer. Generics make healthcare more affordable, but they’re often made in fewer facilities, sometimes in countries with looser oversight. A single quality issue in one overseas plant can ripple across the entire U.S. and Canadian market. That’s why some people notice differences in how a generic pill works—even if it’s chemically identical. Small changes in fillers or manufacturing processes can affect absorption, especially for drugs with narrow therapeutic windows like levothyroxine or warfarin.
And then there’s the issue of transparency. Most patients have no idea where their meds come from. A 2023 FDA report found that over 80% of active pharmaceutical ingredients in U.S. prescriptions are made abroad, mostly in India and China. The supply chain is optimized for cost, not resilience. When a storm hits a port, a labor strike shuts down a warehouse, or a regulatory audit halts production, it’s the patient who pays the price.
But it’s not all risk. The system also works well most of the time. Pharmacists check for drug interactions, distributors track expiration dates, and regulatory agencies audit facilities. Still, small failures happen more often than you think. That’s why posts here cover topics like how to read pharmacy allergy alerts, why generic vs. brand drugs might behave differently long-term, and how medications like cyclophosphamide or levothyroxine need precise handling to stay effective. These aren’t just medical questions—they’re supply chain questions too.
What you’ll find below are real stories and data-backed insights into how drugs move, fail, and sometimes save lives. From how tanning beds affect skin meds to why fasting changes how your pills work, every post ties back to one truth: the medicine you take doesn’t just appear. It travels. And if you understand how it got there, you can protect yourself better.
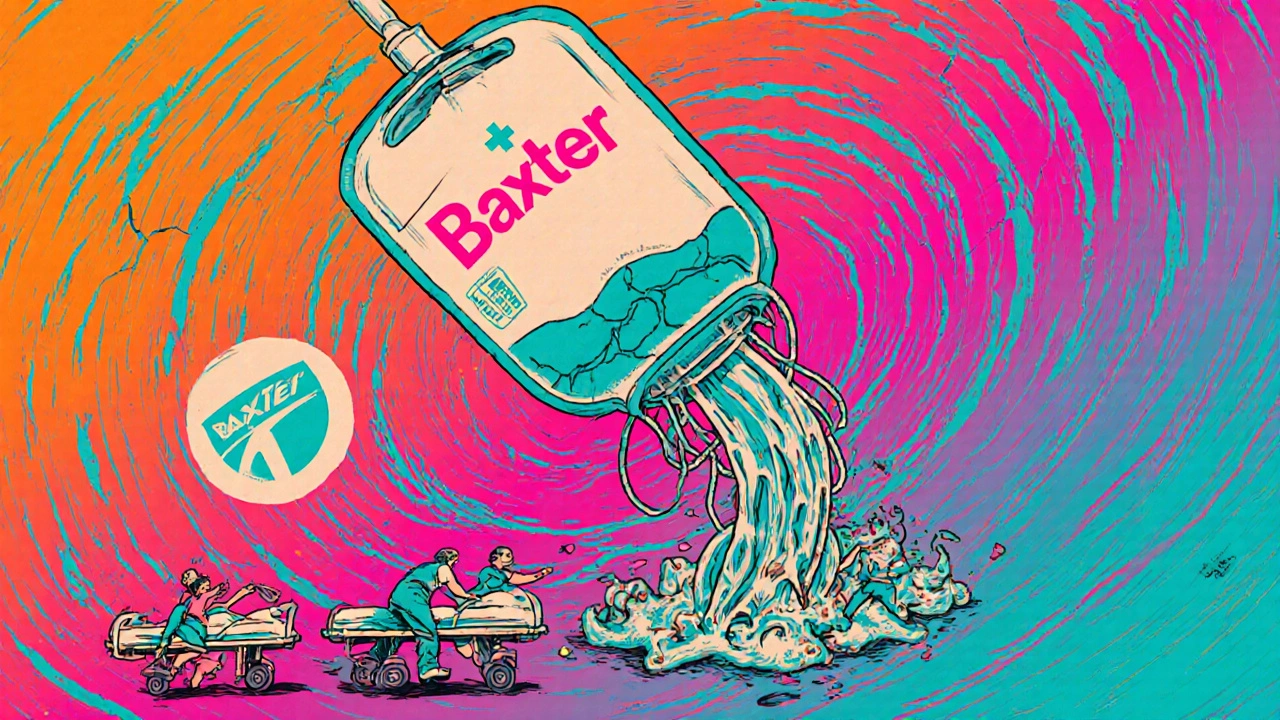
Natural Disasters and Drug Shortages: How Climate Change Is Disrupting Medicine Supply
Nov, 30 2025
Natural disasters like hurricanes and floods are increasingly causing life-threatening drug shortages across the U.S. From IV fluids to insulin, climate risks are exposing dangerous gaps in the pharmaceutical supply chain-and patients are paying the price.
Long-Term Solutions for Building Resilience into the Drug Supply Chain
Nov, 19 2025
Drug shortages are a growing crisis caused by fragile global supply chains. Learn how targeted domestic production, supplier diversification, AI, and policy changes are building long-term resilience to ensure patients get the medicines they need.