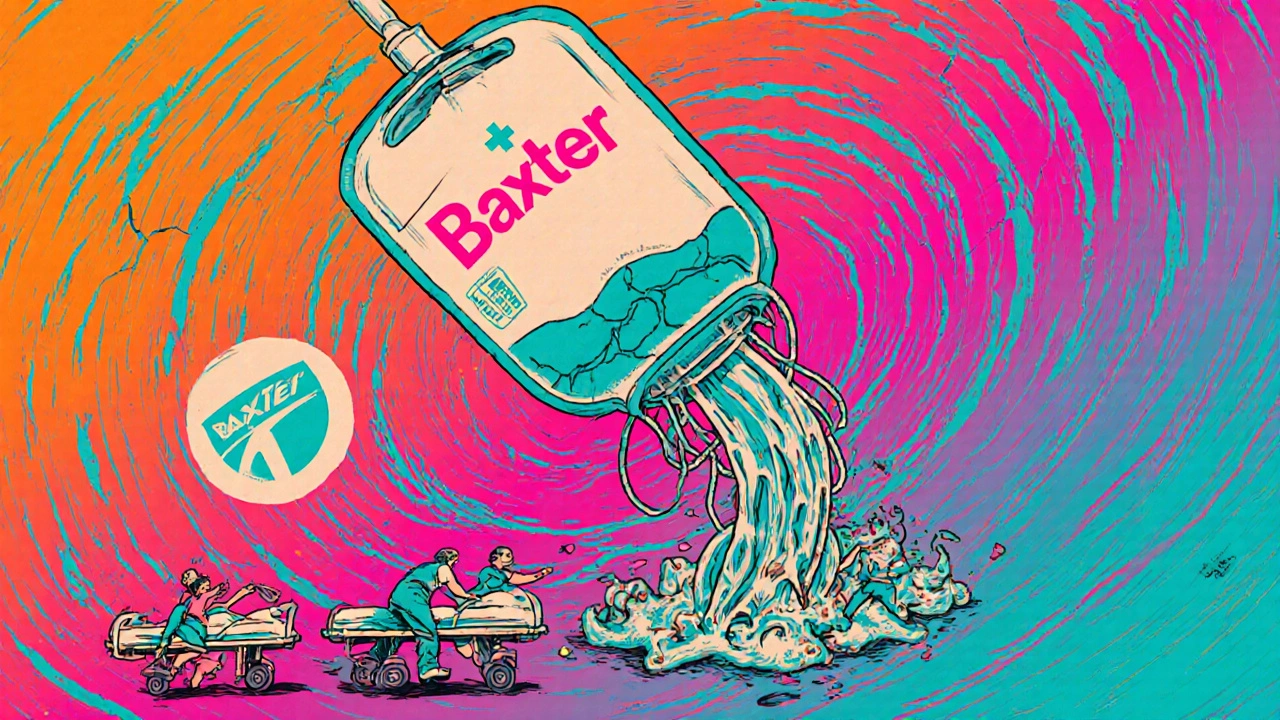
When Hurricane Helene hit North Carolina in September 2024, it didn’t just knock out power and flood homes-it triggered a nationwide medical emergency. One plant, owned by Baxter International, stopped producing 1.5 million bags of IV fluids every day. That’s 60% of the entire U.S. supply. Hospitals scrambled. Elective surgeries were canceled. Cancer patients waited. Nurses rationed fluids. And for many, the reason wasn’t a lack of money or poor planning-it was a storm.
Why a Single Storm Can Shut Down Medicine for Millions
The U.S. pharmaceutical system isn’t built to handle weather. It’s built for efficiency. Factories are clustered in places like Puerto Rico and Western North Carolina because it’s cheap, convenient, and easy to manage. But that also means one hurricane, one flood, or one tornado can knock out half the country’s supply of a life-saving drug. Hurricane Maria in 2017 showed how dangerous this is. Puerto Rico produced 10% of all FDA-approved drugs and 40% of sterile injectables. When the power grid collapsed, it took 11 months to fix. Insulin shortages lasted 18 months. Saline solution? Gone for 14 months. Hospitals had to choose who got fluids and who didn’t. That’s not a glitch. That’s how the system works. Today, 65.7% of all U.S. drug manufacturing facilities sit in counties that have had at least one federal weather disaster declaration since 2018. Hurricanes are the biggest threat-responsible for nearly half of all climate-related drug disruptions. But floods, wildfires, and even extreme heat are catching up. In 2022, flooding in Michigan hit Abbott’s infant formula plant during an already critical shortage. The result? Eight more weeks of empty shelves for babies across the country.The Hidden Weak Spots in Your Medicine Cabinet
It’s not just about big names like insulin or saline. It’s about the small, quiet drugs you never think about until you need them. - 78% of sterile injectable drugs in the U.S. have only one or two manufacturing sites. If that one site goes down, there’s no backup. - 90% of the ultra-pure quartz used in medical devices comes from one town in North Carolina-Spruce Pine. A single landslide or storm could disrupt heart monitors, ventilators, and dialysis machines. - Generic drugs, the cheapest and most widely used, are the most vulnerable. They’re made in low-margin, high-volume plants with little room for error or investment in backup systems. The FDA now tracks natural disasters as a top cause of drug shortages. Between 2017 and 2024, climate events caused 32% of all interruptions. That’s more than raw material shortages, regulatory delays, or factory recalls. It’s the weather. And it’s getting worse. NOAA predicts a 25-30% increase in Category 4 and 5 hurricanes by 2030. That means more storms hitting the same high-risk zones. More shutdowns. More delays. More patients left without treatment.Why Just-in-Time Doesn’t Work When the Power’s Out
The pharmaceutical industry runs on just-in-time inventory. That means drugs are made, shipped, and sold with almost no extra stock. It saves money. It sounds smart. But it’s a disaster waiting to happen. When Hurricane Helene hit, Baxter’s plant went offline. Within 72 hours, hospitals were running out of IV fluids. It took weeks for the FDA to approve emergency imports from Europe. By then, damage was done. Patients missed treatments. Recovery times lengthened. Some didn’t make it. Why didn’t they have backups? Because it’s expensive. Building a second plant for the same drug can cost $500 million. And if you’re making a generic drug that sells for $1 a bag, who’s going to pay for that? The answer: no one-until it’s too late. Hospitals tried to stretch supplies. Some reused IV bags. Others extended expiration dates. But that took hours of pharmacy staff time per drug. Nurses were already stretched thin. Pharmacists worked 16-hour days. And still, it wasn’t enough.
What’s Being Done-and Why It’s Not Enough
There are signs of change. The FDA launched a Critical Drug Resilience Program in January 2025. It fast-tracks approval for manufacturers who spread production across three climate-resilient regions. That’s a start. The Strategic National Stockpile now pilots emergency stockpiles of critical injectables in hurricane zones. During Helene, those reserves cut shortage duration by 40% compared to Maria. That’s progress. Some companies are using AI to predict disasters. Sensos.io flagged Helene’s impact on IV fluid supply 14 days ahead of time. A few hospitals used that warning to stockpile extra fluids. They were ready. Others weren’t. But here’s the problem: only 31% of top pharmaceutical companies have actually implemented meaningful resilience strategies. Most still rely on the same risky, centralized model. And regulatory changes? The FDA’s proposed 2025 rule would require manufacturers to keep 90-day emergency inventories of critical drugs. That’s good. But it’s also going to raise drug prices by 4-7%. Will patients pay more? Will insurers cover it? No one knows.Who Gets Left Behind
Big hospitals with 500+ beds are 3.2 times more likely to map their supply chains and prepare for disruptions. Smaller clinics? Rural hospitals? Community pharmacies? They don’t have the staff, the money, or the tech. When a storm hits, they’re the last to get help-and the first to run out. Cancer patients are especially at risk. Older generic injectables-like those used in chemotherapy-are already in chronic shortage. Natural disasters make it worse. The American Cancer Society says climate-related disruptions are now a major reason patients miss treatments. That’s not a side effect. That’s a failure of the system. And it’s not just the U.S. The 2018 earthquake in Iran killed 700 people and injured 10,000. But because Iran’s drug production is more spread out, the medical supply didn’t collapse. The U.S. system, by contrast, is fragile because it’s too concentrated.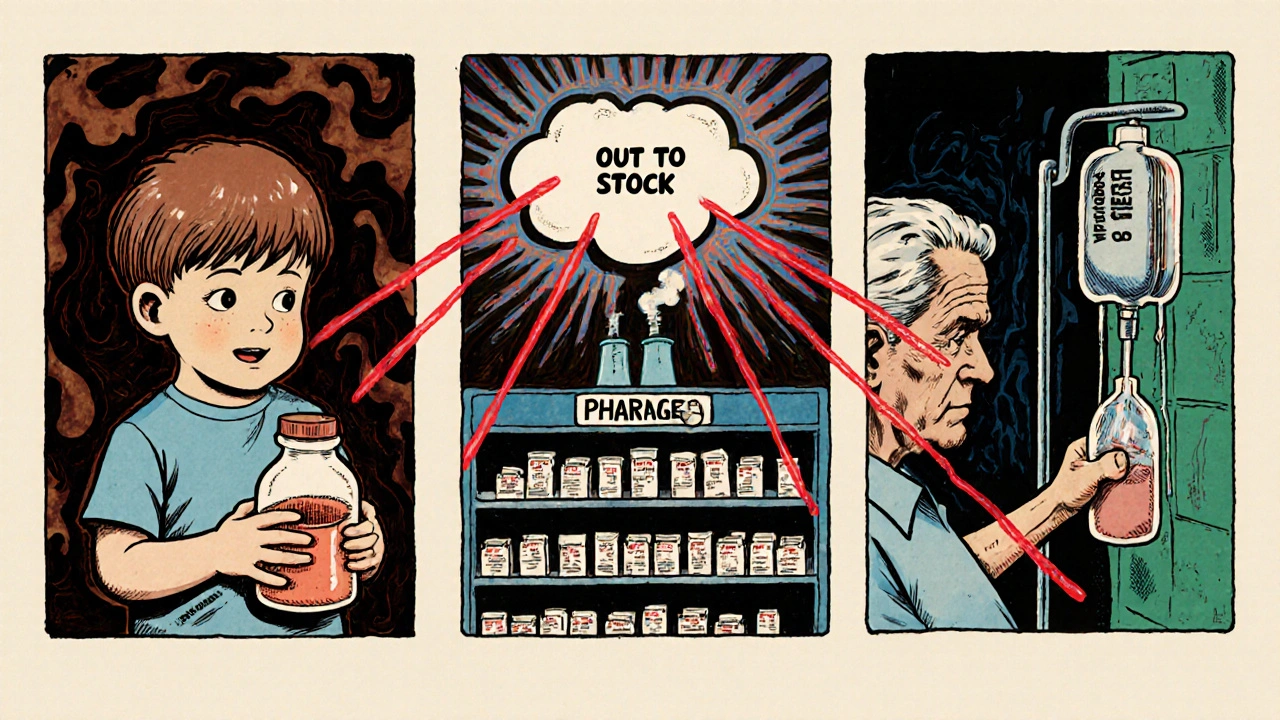
What Needs to Happen Now
We can’t stop hurricanes. We can’t stop climate change. But we can stop pretending the current system will hold up. - Build redundancy. Every critical drug needs at least two manufacturing sites in different regions. Not just for cost-but for survival. - Stockpile wisely. Emergency reserves of saline, insulin, antibiotics, and anesthetics should be mandatory in high-risk zones. Not optional. Not after the fact. - Force transparency. Manufacturers must disclose where their drugs are made, what suppliers they rely on, and what climate risks they face. No more hiding behind trade secrets. - Protect small providers. Federal aid and tech tools must reach rural clinics and community pharmacies. They can’t be left to fend for themselves. The cost of doing nothing is measured in lives. Every delay in chemotherapy. Every postponed surgery. Every IV bag rationed. That’s not just a supply chain issue. It’s a public health crisis.What You Can Do
You can’t rebuild a factory. But you can stay informed. If you rely on a medication that’s often in short supply-like insulin, saline, or chemotherapy drugs-talk to your pharmacist. Ask:- Is there a backup brand or formulation?
- Do we have a supply on hand if a storm hits?
- Has the pharmacy signed up for emergency alerts from the FDA or state health department?
Can climate change really cause drug shortages?
Yes. Between 2017 and 2024, climate-related events caused 32% of all U.S. drug shortages. Hurricanes, floods, and wildfires have shut down key manufacturing plants, leading to nationwide shortages of insulin, IV fluids, antibiotics, and chemotherapy drugs. The 2017 Hurricane Maria disaster alone disrupted 10% of all FDA-approved drugs.
Which drugs are most at risk during natural disasters?
Sterile injectables like saline solution, insulin, antibiotics, and chemotherapy drugs are the most vulnerable. These drugs are often made in just one or two facilities. Generic drugs are especially at risk because they have low profit margins, making it harder to invest in backup systems. IV fluids, which are critical for surgery, hydration, and medication delivery, are among the most frequently affected.
Why don’t drug companies just make more in different places?
Building a new pharmaceutical facility costs $500 million or more. For generic drugs, which sell for pennies per dose, there’s little financial incentive. The industry relies on centralized, low-cost manufacturing. This model works until a storm hits. Then, there’s no backup. Some companies are starting to diversify, but progress is slow.
Are there emergency supplies of drugs during disasters?
Yes, but they’re limited. The Strategic National Stockpile now holds emergency reserves of critical injectables in hurricane-prone areas. During Hurricane Helene in 2024, these reserves cut shortage duration by 40% compared to Hurricane Maria in 2017. But coverage is still patchy, and most hospitals don’t have access to these stockpiles unless they’re in a designated high-risk zone.
What’s being done to fix this problem?
The FDA launched the Critical Drug Resilience Program in January 2025 to fast-track approval for manufacturers who spread production across three climate-resilient regions. New rules in 2025 will require manufacturers of critical drugs to keep 90-day emergency inventories. AI tools are also being used to predict disruptions. But only 31% of top pharmaceutical companies have implemented real resilience strategies. Most still rely on the same risky, centralized system.
How can patients protect themselves from drug shortages?
If you rely on a drug that’s often in short supply, ask your pharmacist: Is there a backup version? Do we have extra on hand? Have we signed up for FDA emergency alerts? Keep a 30-day supply if you can. Stay informed about weather risks in your region. And if you’re a caregiver or advocate, push local health officials to include drug supply planning in disaster preparedness.
By 2030, experts predict climate-related drug shortages could increase by 150%. That’s not a forecast. It’s a warning. The medicine you need might be one storm away from being gone. The system isn’t broken-it was never built to survive this.
James Allen
December 1, 2025 AT 17:46Let’s be real-this isn’t about climate change. It’s about China and India running the global pharma supply chain while we sit here like helpless toddlers waiting for our medicine to arrive. We built this mess by outsourcing everything because it was cheaper. Now we’re crying because the storm hit? Wake up. We had decades to fix this. We chose not to. Now we pay the price.
Kelly Essenpreis
December 3, 2025 AT 00:10the whole thing is a scam
Lauryn Smith
December 4, 2025 AT 08:50I work in a rural clinic. We got hit with an IV fluid shortage last winter after a snowstorm knocked out power for three days. We had to mix saline from concentrate because we had zero backup. No one came to help. No one even asked if we were okay. This isn’t theoretical. It’s happening to real people every day.
Mary Ngo
December 5, 2025 AT 09:18Have you considered that this isn’t just about weather-it’s about the deliberate dismantling of domestic manufacturing under the guise of neoliberal efficiency? The same people who pushed for deregulation and offshoring are now pretending to be shocked when their ideology collapses under the weight of a hurricane. This is a manufactured crisis, engineered by corporate lobbyists who profit from fragility. The FDA’s ‘resilience program’? A PR stunt. The 90-day inventory rule? Too little, too late. They want you to believe this is an accident. It’s not. It’s a feature.
And don’t get me started on the ‘transparency’ demand. You think they’ll ever reveal their supply chains? The same ones that source quartz from North Carolina while secretly outsourcing active pharmaceutical ingredients to factories in Bangladesh with zero climate safeguards? The system isn’t broken-it’s functioning exactly as designed. To profit. To obscure. To sacrifice the vulnerable for quarterly earnings.
And yet, here we are, debating whether to stockpile saline while the CEOs fly to their private islands in the Caribbean. The moral bankruptcy is staggering. We’re not just failing patients-we’re failing our own humanity. This isn’t policy. It’s necropolitics.
And you know what’s worse? The fact that most people don’t even care until their mother can’t get her chemo. Then suddenly, it’s urgent. Then suddenly, they want answers. But by then, it’s too late. The system doesn’t care about your mother. It cares about margins. And it will always choose margins over lives.
Edward Hyde
December 6, 2025 AT 09:36Oh wow, another ‘climate is the real villain’ sob story. Newsflash: the real villain is the FDA’s archaic approval process and the unions that make it impossible to build new plants without a 12-year bureaucratic odyssey. You think a hurricane’s the problem? Try getting a permit to pour concrete in a hurricane zone without 47 environmental impact studies, 19 public hearings, and a committee of bureaucrats who think ‘resilience’ means painting the building green. We don’t need more stockpiles-we need less red tape. But no, let’s just keep blaming the weather while the real culprits sip lattes in DC.
Amber-Lynn Quinata
December 6, 2025 AT 12:35My dad’s on chemo. We’ve had to switch brands twice in the last year because of ‘supply issues.’ Last month, the pharmacy said they might not get his next dose for 3 weeks. I cried in the parking lot. I’m not mad at the weather. I’m mad at the people who knew this was coming and did nothing. 🥺
Kenny Leow
December 6, 2025 AT 15:18As someone who grew up in Puerto Rico after Maria, I can tell you this isn’t new. We lost power. We lost medicine. We lost people. And now the mainland acts like this is a surprise? We’ve been screaming into the wind for years. The U.S. treats Puerto Rico like a backup generator-useful until it breaks, then ignore it. If you want resilience, stop outsourcing to disaster zones and start investing in real infrastructure-everywhere. Not just where it’s profitable.
And yes, I’m still mad. 😔
Alexander Williams
December 6, 2025 AT 22:37The systemic vulnerability stems from concentration risk in the upstream manufacturing ecosystem, particularly in the production of sterile injectables and API intermediates. The elasticity of supply is functionally zero under exogenous shock events due to the absence of parallelized production topology. The FDA’s 90-day inventory mandate is a necessary but insufficient intervention-what’s required is a decentralized, multi-hub supply architecture with geographically dispersed critical material sourcing. Without modular redundancy and real-time supply chain telemetry, we’re merely delaying the next systemic failure.