Why Timing Matters When You're on Immunosuppressants
If you're taking drugs like methotrexate, rituximab, or TNF inhibitors, getting vaccinated isn't as simple as walking into a clinic and saying "I'm due." These medications weaken your immune system on purpose - to stop your body from attacking your joints, organs, or cancer cells. But that same suppression makes it harder for your body to respond to vaccines. The result? You might get a shot and still not build enough protection. That’s not just a risk - it’s a real danger during flu season, RSV outbreaks, or when new variants emerge.
The goal isn’t to stop your treatment. It’s to time your vaccines so they actually work. Studies show that people who get vaccines too close to starting or restarting immunosuppressants have up to 60% lower antibody levels. That’s not a small difference. It’s the difference between being protected and being vulnerable.
When to Get Vaccinated Before Starting Immunosuppressants
The clearest rule across all major guidelines is this: get vaccinated before you start immunosuppressive therapy. The CDC says at least 14 days before. But that’s the bare minimum. Most specialists recommend 2 to 4 weeks, and for some drugs, even longer.
For example, if you’re about to begin rituximab - a drug that wipes out B-cells - experts say you need to be fully vaccinated at least 6 months before your first dose. Why? Because once those B-cells are gone, they don’t come back quickly. Your body can’t make new antibodies for months, sometimes over a year. Waiting 6 months isn’t overcautious - it’s based on real data showing vaccine responses drop to near zero after just one cycle of rituximab.
Same goes for other B-cell depleting drugs like ocrelizumab or ofatumumab. If you’re on one of these for MS, lupus, or rheumatoid arthritis, don’t wait until you’re already on the drug to schedule your shingles or pneumonia shots. Do it before you start. Many patients don’t realize this until they’re already on treatment and then find out they missed their window.
What to Do If You’re Already on Immunosuppressants
It’s not all lost if you’re already taking immunosuppressants. But you need to know which drugs you’re on and how they interact with vaccines.
For drugs like azathioprine, mycophenolate, or cyclophosphamide - which slow down immune cells broadly - you can usually get non-live vaccines (like flu, COVID, or Hepatitis B) without stopping them. But live vaccines? That’s different. The shingles vaccine (Shingrix) is not live, so it’s safe. But the old chickenpox vaccine (Varivax) is live. You can’t get that if you’re on these drugs. Ever. The risk of the vaccine causing infection is real.
For biologics like TNF inhibitors (Humira, Enbrel, Cimzia), the American College of Rheumatology says hold the drug for one dose before vaccination and wait four weeks after. This gives your immune system a short window to respond. Studies show this increases antibody production by about 25% compared to not pausing.
Methotrexate is a special case. If you’re on it for arthritis and it’s working well, your doctor might ask you to skip one or two doses after your flu shot. A 2022 trial found that patients who paused methotrexate for two weeks after vaccination had a 27% higher chance of developing protective antibodies. That’s not a guess - that’s from three randomized trials. It’s one of the few times we have solid proof that timing changes outcomes.
How Long to Wait After Stopping Immunosuppressants
Stopping your meds doesn’t mean your immune system snaps back to normal overnight. Recovery takes time - and it varies by drug.
For most oral drugs like methotrexate or leflunomide, waiting 4 weeks after your last dose is usually enough. But for drugs that wipe out immune cells, like rituximab, you need to wait much longer. The IDSA 2025 draft guidelines say 3 to 6 months after your last dose before getting most vaccines. Why? Because your body needs time to rebuild its B-cell population. Some people take 9 months or more. That’s why doctors now check your blood for B-cell counts before giving vaccines - not just the calendar.
IVIG therapy is another curveball. If you’ve had high-dose IVIG (like 2 grams per kilogram), you need to wait 11 months before getting a live vaccine. Why? Because the antibodies in the IVIG can neutralize the vaccine before your body even has a chance to respond. That’s not a myth - it’s written in the guidelines from the American College of Rheumatology and backed by real-world case data.
Conflicting Guidelines - Why Doctors Disagree
You might hear different advice from your rheumatologist, oncologist, or primary care doctor. That’s because guidelines aren’t all the same.
The CDC says 14 days before starting immunosuppressants. The American Society of Hematology says 2 to 4 weeks. The European League Against Rheumatism says 7 to 10 days. The ACR says 6 months after rituximab. IDSA says 3 to 6 months. None of them are wrong - they’re just looking at different patient groups, different risks, and different evidence.
One study in the Journal of Rheumatology found that 68% of rheumatologists struggle to pick the right timing because the guidelines conflict. And it’s not just doctors - patients are confused too. Reddit threads are full of people asking, "Why did my oncologist say I can get the vaccine now, but my rheumatologist says I have to wait six more months?"
The truth? There’s no one-size-fits-all answer. Your age, the disease you have, how long you’ve been on the drug, and even your blood test results all matter. That’s why personalized timing is becoming the new standard.
What You Can Do Right Now
You don’t need to wait for your doctor to bring this up. Take control.
- If you’re planning to start immunosuppressants, ask your doctor: "What vaccines do I need before I start?" Get them done at least 4 weeks before, if possible.
- If you’re already on treatment, ask: "Which of my meds affect vaccines? Should I pause any before my next shot?" Don’t assume your pharmacist or nurse knows your full med list.
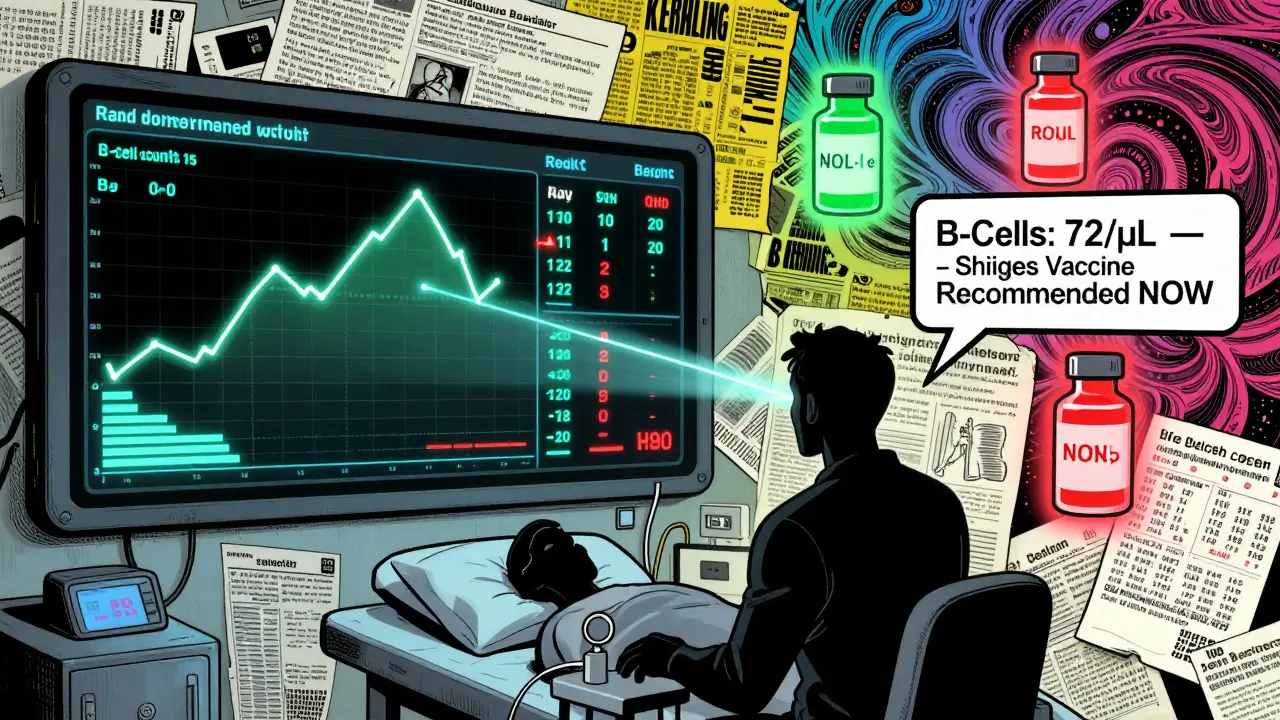
- Ask for a B-cell count test if you’re on rituximab or similar drugs. A count above 50 cells/μL is a good sign your immune system is ready.
- Use the free Immunosuppressant-Vaccine Timing Calculator from UCSF. It’s built into some hospital portals and available online. Plug in your meds and it tells you the safe window.
Don’t skip vaccines because you’re afraid of flaring your disease. Yes, pausing meds can cause a flare - about 31% of patients report it. But the risk of getting sick with something preventable - like pneumonia or flu - is far higher. Work with your doctor to find the safest balance.
The Future: Personalized Timing Is Coming
Fixed timelines are fading. The future is biomarkers.
The NIH is running a study called VAXIMMUNE, tracking 2,500 people on immunosuppressants. Instead of saying "wait 6 months," they’re measuring your actual immune response - T-cell counts, antibody levels, B-cell recovery - and timing vaccines based on your body’s signals. Early results show this approach boosts protection by 40% compared to fixed schedules.
Big health systems like Epic are building tools into electronic records that will auto-suggest vaccine timing based on your meds. By 2025, your doctor’s computer might pop up: "Patient on rituximab - last dose 8 months ago. B-cell count: 72/μL. Recommended: Shingles vaccine now."
This isn’t sci-fi. It’s happening. And it means the days of guessing, waiting, and hoping your vaccine worked are ending. The goal is no longer just to give you a shot - it’s to make sure your body actually responds.
What to Do If You Got Sick After a Vaccine
If you got a vaccine and still got sick - flu, COVID, shingles - don’t blame yourself. You did everything right. The problem isn’t you. It’s that your immune system was too suppressed to respond.
That’s why experts now say: if you’re on immunosuppressants and you get a vaccine, you should still get boosted. And you should consider extra layers of protection - like Evusheld (if available), monoclonal antibodies, or even prophylactic antivirals during outbreaks.
One patient on Reddit wrote: "I waited 6 months after rituximab for the shingles shot. Got it. Still got shingles. My doctor said it was ‘expected.’ That doesn’t feel like care - it feels like resignation."
That’s the reality. Vaccines aren’t perfect for everyone on immunosuppressants. But they’re still the best tool we have. And timing them right? That’s the only way to give them a fighting chance.
Can I get the flu shot while on methotrexate?
Yes, you can. But studies show you’re more likely to develop strong protection if you pause methotrexate for two weeks after the shot. This isn’t required for everyone, but if your arthritis is stable, skipping one or two doses can boost your antibody response by nearly 30%. Talk to your rheumatologist about whether it’s safe for you.
Do I need to wait before getting the COVID vaccine if I’m on rituximab?
Yes. Most guidelines recommend waiting at least 6 months after your last rituximab dose before getting any vaccine, including COVID. This is because rituximab wipes out the immune cells that make antibodies. Getting vaccinated too soon means your body can’t respond. Some doctors will check your B-cell count first - if it’s above 50 cells/μL, they may allow the shot earlier. Don’t assume the 6-month rule is absolute - ask for testing.
Is it safe to get a live vaccine like MMR or chickenpox while on immunosuppressants?
No. Live vaccines - including MMR, varicella (chickenpox), and the old version of the shingles vaccine (Zostavax) - should never be given to people on immunosuppressants. Even if you’re not on the strongest drugs, the risk of the vaccine causing infection is real. Stick to non-live vaccines like Shingrix, which is safe and effective.
What if I missed my window and started immunosuppressants before getting vaccinated?
It’s not too late, but your options are limited. You can still get non-live vaccines like flu, COVID, and pneumonia - but they may not work as well. Your doctor may recommend extra doses (like a third or fourth COVID shot) or antibody treatments like Evusheld. You’ll also need to be extra careful about avoiding exposure to illness. The goal now is damage control - not prevention.
Why do some doctors say to wait 2 weeks and others say 6 months?
Because not all drugs are the same. For most oral meds like methotrexate, 2-4 weeks is enough. But for drugs that destroy immune cells - like rituximab, ocrelizumab, or high-dose chemotherapy - it takes months for your body to rebuild. A 2-week wait won’t help if your B-cells are gone. The difference comes down to the type of drug, not the doctor’s opinion. Ask which class your medication belongs to.
Nancy Nino
February 1, 2026 AT 08:39Wow. Just... wow. I’ve been on methotrexate for six years and never once had a doctor mention pausing doses after a flu shot. I thought they just didn’t work well-I didn’t realize I was *actively sabotaging* my immune response. This is the kind of info that should be printed on prescription bottles. Thank you for writing this. I’m scheduling my B-cell count test tomorrow.
Deep Rank
February 3, 2026 AT 04:31ok so i read this whole thing and like… i think u r right but also? what if u r just a glorified pharmacy bot? like i got my covid shots while on rituximab and i was fine?? i mean i got sick but that was bc my cat sneezed on me?? also i dont trust guidelines from america they dont even have good tea here. also my cousin in delhi got her shingles shot 3 weeks after her last dose and she’s fine?? so maybe u r just scaring ppl for clicks??
Ishmael brown
February 3, 2026 AT 12:46💀 I’m crying. Not because I’m moved-because I just realized I got my shingles shot 3 months after rituximab and now I’m basically a walking petri dish. I’m 42. I have two kids. And I just got a 10-minute lecture from my rheumatologist while she checked her phone. I’m not mad. I’m just… disappointed. Like, I paid $200 for this vaccine. I deserve more than a shrug.
Aditya Gupta
February 3, 2026 AT 16:23Good stuff. Real talk: if you're on immunosuppressants, your body is doing a marathon with weights. Vaccines are your water bottle. Timing = survival. Don't wait for your doctor to tell you. Ask. Push. Bring this article. We need more people like you speaking up.
Lisa Rodriguez
February 4, 2026 AT 07:50My rheumatologist told me to wait 4 weeks after stopping methotrexate before my flu shot. I did. Got my antibodies tested. They were barely detectable. So I got another shot. And then another. Now I’m on my fourth dose. It’s exhausting. But I’m alive. And I’m not letting this disease win. If you’re on these meds, don’t give up. Keep asking. Keep pushing. You’re not being difficult-you’re being smart.
Ed Di Cristofaro
February 4, 2026 AT 15:59People like you make me sick. You think if you just wait 6 months and get a blood test everything’s fine? What about the people who can’t afford to stop their meds? Who can’t take time off work? Who don’t have a doctor who gives a damn? You’re not helping. You’re just making guilt trips for people who are already drowning.
Lilliana Lowe
February 5, 2026 AT 08:37While the general thrust of this post is commendable, one must note the conspicuous absence of peer-reviewed meta-analyses cited in support of the 6-month rituximab window. The IDSA draft guidelines referenced are, as of this writing, unpublished. Moreover, the claim that ‘antibody levels drop to near zero’ lacks quantitative anchoring-zero relative to what baseline? Healthy controls? Pre-treatment titers? The absence of precise metrics undermines the entire argument. This is not science; it’s medical folklore dressed in HTML.
vivian papadatu
February 6, 2026 AT 11:00I’m from a small town in rural Tennessee. My doctor doesn’t even know what rituximab is. I had to print this article and hand it to him. He said, ‘Huh. I’ll look into it.’ Two weeks later, he called me back: ‘We’re doing the B-cell test.’ I cried in the parking lot. This isn’t just about vaccines. It’s about being heard. Thank you for giving people like me the words to speak.
Bob Cohen
February 7, 2026 AT 00:05So… I’m on Humira. Got my flu shot last week. My doc said skip one dose before and wait four weeks after. I did. Still got the flu. 😅 But I didn’t end up in the hospital. So… I guess that’s a win? I’m just glad I didn’t skip it. I’ve seen what happens when people skip. It’s not pretty. Thanks for the reminder-timing isn’t magic, but it’s the best shot we’ve got.
Chris & Kara Cutler
February 7, 2026 AT 11:52My husband’s on methotrexate. We paused his dose after his flu shot. He felt weird for two days. But he didn’t get sick. And his titers were 3x higher than last year. 🙌 We’re doing it again next time. You’re not being a burden-you’re being brave.
Rachel Liew
February 7, 2026 AT 20:21i read this and i just wanted to say thank you. my mom is on rituximab and she was so scared to get the vaccine because she thought it would make her sicker. i showed her this. she cried. then she called her doctor. she got her b-cell test. she’s getting her shot next week. you helped us. thank you.
Jamie Allan Brown
February 7, 2026 AT 22:58There’s a quiet revolution happening here. We’re moving from one-size-fits-all medicine to personalized immune mapping. This isn’t just about vaccines-it’s about dignity. The fact that we’re now measuring B-cells instead of just counting days? That’s progress. I’ve seen patients die because they were told to wait ‘a few weeks.’ This post? It’s a lifeline. Keep sharing it.
Nicki Aries
February 8, 2026 AT 19:52Let me just say this: If you’re not asking your doctor about vaccine timing while on immunosuppressants… you’re not advocating for yourself. And if your doctor doesn’t know the difference between methotrexate and rituximab? Find a new one. This isn’t optional. This is your life. You deserve better than a 3-minute consult and a printed CDC pamphlet. I’m not being dramatic. I’m being real.