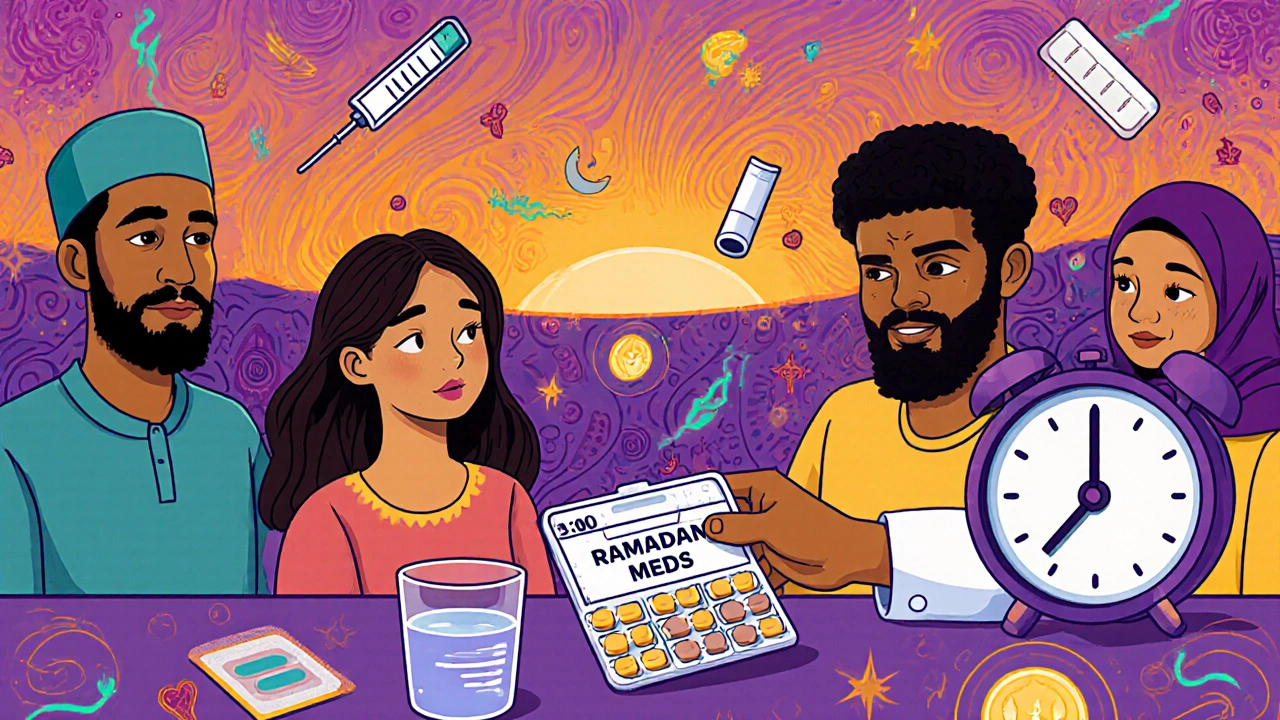
Ramadan Medication: What You Need to Know About Taking Pills During Fasting
When you're fasting during Ramadan, the holy month of Islamic fasting where food and drink are avoided from dawn to sunset. Also known as sawm, it's a spiritual practice that millions follow each year. But what happens when you're also taking medication? Many people assume they must stop their prescriptions during daylight hours—but that’s not always true, and sometimes it’s dangerous. Medication timing, the schedule you take your pills in relation to meals and daily routines changes dramatically during Ramadan, and that shift can affect how well your drugs work—or cause side effects.
Not all medications break your fast. Pills, capsules, and patches usually don’t, because they’re not food or drink. But some drugs, like liquid syrups or chewable tablets, might be seen differently by religious scholars, depending on how they’re used. Drug absorption, how your body takes in and processes medicine is also affected when you’re not eating. For example, thyroid medication like levothyroxine needs an empty stomach to work right, and fasting might actually help with that—but only if you take it at the right time. On the other hand, medicines that irritate your stomach, like certain antibiotics or painkillers, can cause problems if taken without food. Even something as simple as a daily vitamin or supplement might need to be rescheduled.
People with chronic conditions—like diabetes, high blood pressure, epilepsy, or depression—often need to adjust their treatment plans during Ramadan. Some may switch from three doses a day to two, taking one at Suhoor (pre-dawn meal) and one at Iftar (evening meal). Others might need to change the type of medication entirely. For instance, extended-release pills are often better than immediate-release ones during fasting, because they reduce the number of doses needed. But you can’t just guess what works. You need to talk to your doctor or pharmacist, ideally weeks before Ramadan starts. They can check your current meds against fasting guidelines, look at your health history, and help you avoid dangerous drops in blood sugar, spikes in blood pressure, or missed doses that lead to seizures or relapses.
There’s also the issue of hydration. Some drugs, like diuretics or those for kidney disease, increase fluid loss. If you’re not drinking water during the day, you could end up dehydrated or with electrolyte imbalances. And if you’re taking something like opioid therapy, a treatment for severe pain that carries risks of dependence and side effects, fasting might make dizziness or nausea worse. Even mental health meds, like antidepressants, drugs used to treat mood disorders by balancing brain chemicals, can behave differently if your sleep and eating patterns shift. The body’s internal clock affects how drugs are metabolized—and fasting changes that clock.
What you’ll find in the posts below are real, practical guides from people who’ve been there. You’ll see how others managed thyroid meds, antibiotics, blood pressure drugs, and even supplements during Ramadan. There are tips on timing, what to ask your doctor, and how to spot warning signs when something’s not working. No fluff. No guesswork. Just clear, tested advice from patients and pharmacists who know what works—and what doesn’t—when you’re fasting and fighting illness at the same time.
Religious Fasting and Medication Timing: Safe Dosing During Fasts
Nov, 16 2025
Learn how to safely manage medications during religious fasting, especially during Ramadan. Discover when to take pills, which drugs are safe, and how to adjust dosing without risking your health.