It’s not uncommon to feel nervous about starting a new medication. You’ve read the list of possible side effects-nausea, dizziness, insomnia, weight gain, low libido-and your mind races: What if this happens to me? What if it never goes away? What if it’s worse than the condition I’m treating? You’re not alone. Around 60% of people on long-term medications report significant anxiety about what might happen next. And here’s the twist: sometimes, the anxiety itself is making the side effects feel worse.
Why Your Mind Makes Side Effects Feel Worse
Your brain is wired to protect you. When you hear a drug might cause fatigue or headaches, your nervous system goes on high alert. You start noticing every tiny ache, every moment of tiredness, and your brain says, That’s the medication. This isn’t weakness-it’s biology. In the 1980s, researchers like Dr. Fabrizio Benedetti identified the nocebo effect: when expecting harm, your body actually produces it. A 2022 meta-analysis found that patients told about potential side effects were significantly more likely to report them-even when they were given a sugar pill.That’s why two people on the same drug can have wildly different experiences. One feels fine; the other is convinced they’re falling apart. The difference? How their mind interprets physical sensations. Anxiety turns normal body changes into red flags. Fatigue from a long day? It’s the antidepressant. A stomach rumble? It’s going to be severe nausea. This cycle keeps people from sticking with treatment-even when the medication is working.
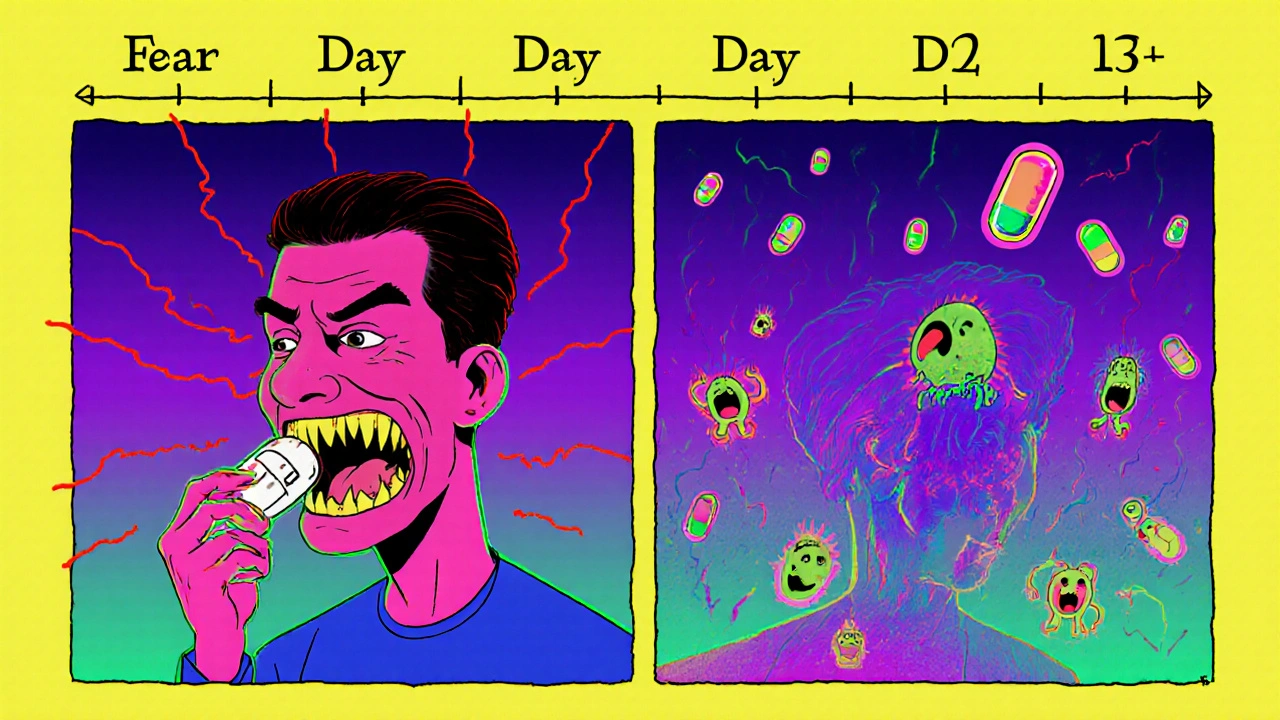
What Actually Happens to Side Effects Over Time
Most side effects aren’t permanent. In fact, the majority fade. For SSRIs-commonly prescribed for anxiety and depression-nausea, dizziness, and fatigue typically peak between days 3 and 5. By day 14 to 21, they’ve dropped by 65-75% in most people, according to Mayo Clinic’s 2024 guidelines. The same goes for blood pressure meds: dizziness often improves within two weeks as your body adjusts.Yet, many people quit before this window closes. A 2021 study in the Journal of Clinical Psychopharmacology showed that when patients were told exactly when side effects would likely improve, adherence jumped by 32%. Knowing the timeline takes the mystery out of discomfort. It’s not a sign the drug is failing-it’s proof your body is adapting.
Three Proven Psychological Tools to Reduce Medication Anxiety
1. Cognitive Restructuring: Challenge the Worst-Case Story
Your brain loves to spin worst-case scenarios: If I get nausea, I’ll vomit all night. If I can’t sleep, I’ll lose my job. If this doesn’t work, I’ll be stuck like this forever. Cognitive restructuring helps you test those stories.Ask yourself:
- What’s the actual chance this will happen? (For most side effects, it’s under 20%.)
- Have I seen this happen to others? Or am I imagining it?
- What’s the evidence this is caused by the drug-not stress, lack of sleep, or coffee?
One patient on Reddit tracked her SSRI side effects for two weeks. She realized her “constant dizziness” only happened after she skipped breakfast. The medication wasn’t the culprit-low blood sugar was. That shift in thinking kept her on treatment.
2. Symptom Normalization: You’re Not Broken
It’s easy to feel like you’re the only one struggling. You’re not. Nearly 70-80% of people on antidepressants experience temporary nausea, headaches, or sleep changes. These aren’t signs of failure-they’re signs your body is adjusting. A 2023 review of 1,243 patient comments found that those who practiced “symptom normalization” (reminding themselves: This is common. This is temporary.) saw a 65% drop in anxiety about their meds.Try this: Write down the side effect you fear. Then write: “This happens to ___% of people on this drug. It usually fades by week 3.” Keep that note on your phone. Read it when panic hits.
3. The Two-Week Rule: Give It Time
Commit to taking your medication for 14 days before deciding whether to stop. Use those two weeks to practice coping tools, not to judge the drug. Set a daily reminder: Day 1 of 14. Track your symptoms in a simple journal-not to obsess, but to spot patterns. Did the dizziness only happen after 2 p.m.? Was the insomnia worse on days you drank coffee? This turns fear into data.One woman in her 40s, featured in Better Health Channel’s patient stories, had tried to quit her SSRI four times in one year. Each time, she stopped after three days of nausea. After using the two-week rule and tracking her symptoms, she realized: the nausea always ended by day 16. She stayed on the medication-and her anxiety improved.
What Works Best: CBT, ACT, and Mindfulness
Not all psychological approaches are the same. Here’s what the data says:| Approach | Effectiveness | Time to See Results | Long-Term Retention |
|---|---|---|---|
| Cognitive Behavioral Therapy (CBT) | 65-75% | 4-6 sessions (2-4 weeks) | 65% at 6 months |
| Acceptance and Commitment Therapy (ACT) | 60-70% | 6-8 sessions (3-5 weeks) | 72% at 6 months |
| Mindfulness-Based Stress Reduction (MBSR) | 50-60% | 8-week program | 68% at 6 months |
| Supportive Therapy | 45-55% | Variable | 50% at 6 months |
CBT is the most studied and gives the fastest results. ACT focuses on accepting discomfort without fighting it-which helps people stay on meds even when symptoms linger. MBSR is great if you can’t access a therapist; an 8-week app-based program can be as effective as six therapy sessions.
What to Do If Your Doctor Dismisses Your Concerns
A 2024 Drugs.com survey found that 42% of people quit their meds because their doctor said, “It’s all in your head.” That’s unacceptable. You’re not imagining your symptoms-you’re experiencing them. But you can still advocate for yourself.Try this script: “I’m not saying the medication isn’t working. I’m asking for help managing the anxiety around the side effects. Can we go over the timeline for improvement? Or recommend a resource on coping strategies?”
If your provider doesn’t respond, ask for a referral to a behavioral health specialist. Many primary care clinics now offer integrated support. Kaiser Permanente, for example, has standardized protocols in 39 centers-and saw a 27% drop in early discontinuations.
When to Consider a Medication Change
Psychological tools help with temporary side effects. But some reactions aren’t normal. If you experience:- Severe chest pain or shortness of breath
- Thoughts of self-harm or suicide
- High fever, confusion, or muscle stiffness (signs of serotonin syndrome)
- Swelling of the face, tongue, or throat
-stop the medication and call your doctor immediately. These aren’t side effects you can “think your way through.”
For milder but persistent issues-like sexual dysfunction or weight gain-talk to your provider about alternatives. Some antidepressants are less likely to cause these. There’s no shame in switching. The goal isn’t to suffer through anything-it’s to find a treatment that works for you.
Tools and Resources You Can Use Today
- SideEffectCope: An FDA-approved app that uses CBT techniques to reduce medication anxiety. In trials, users cut their dropout rates by 53%.
- Mayo Clinic’s Online Guide: Clear, evidence-based info on side effects and coping strategies. Rated 4.7/5 by over 1,200 users.
- “Managing Medication Anxiety” by Dr. Martin Antony: A self-guided workbook with exercises you can do at home. 55% effective when completed over 8 weeks.
- Reddit’s r/mentalhealth: Real stories from people who’ve been there. Search “SSRI side effects” for threads with 2,000+ upvotes.
- Facebook Group: Medication Anxiety Support: Over 14,500 members sharing tips, timelines, and encouragement.
Don’t wait until you’re ready to quit. Start today. Write down one side effect you fear. Write down the timeline for when it usually fades. Then, take your pill.
Medication isn’t the enemy. Fear is. And fear can be managed.

Sammy Williams
November 21, 2025 AT 14:02Man, I wish I'd known this two years ago. I quit my SSRI after three days because I thought the dizziness was gonna kill me. Turns out it was just my brain screaming at me like a alarm clock at 5 AM. Took me another year to work up the courage to try again-and this time, I stuck it out. By day 12, I felt like a new person. Seriously, the two-week rule is real.
Daisy L
November 23, 2025 AT 08:16OMG, YES!! I’ve been screaming this from the rooftops!! My doctor laughed when I said I was ‘fearful of the pills’-like, what, am I a child?? I tracked my nausea in a spreadsheet, labeled it ‘phantom side effects,’ and started drinking ginger tea. Guess what? The nausea vanished-BUT ONLY AFTER I STOPPED PANICKING. The drug didn’t change. MY BRAIN DID. Also, I now have a tattoo that says ‘NOT ALL ACHES ARE DRUGS’-it’s glittery. Deal with it.
Julia Strothers
November 24, 2025 AT 21:14Let me guess-Big Pharma paid you to write this. You know they’ve been suppressing the truth about SSRIs since the 90s, right? The ‘side effects fade’ narrative? A distraction. The real issue is that these drugs alter your neurochemistry permanently. I’ve seen people turn into zombies. I’ve seen families broken. This isn’t ‘anxiety’-it’s chemical enslavement. And now they want you to ‘journal your fears’ while they profit off your dependence. Wake up.
Erika Sta. Maria
November 26, 2025 AT 01:31uuhh… i think this is wrong? i mean, like, in india, we dont even use these pills, we use ayurveda and yoga and chanting ommm. also, the whole ‘nocebo effect’ is just western science being arrogant. my cousin took fluoxetine for 2 years and she became a robot. also, i read on quora that serotonin syndrome is just a myth invented by doctors to sell more meds. also, i dont think your ‘two week rule’ works because time is an illusion anyway. namaste.
Nikhil Purohit
November 26, 2025 AT 09:18Hey, this is actually really helpful. I’ve been on an SNRI for 3 months and I was about to quit because of the insomnia. But after reading this, I checked my sleep log-turns out the worst nights were the ones I drank matcha after 4 PM. I cut that out, kept taking the pill, and now I’m sleeping fine. The key is not blaming the med right away. It’s about patterns. Thanks for the real talk.
Debanjan Banerjee
November 27, 2025 AT 19:22While the psychological strategies outlined here are evidence-based and clinically validated, it is imperative to acknowledge that individual variability in pharmacokinetics and psychosocial context significantly modulates outcomes. The nocebo effect, as documented in the meta-analysis by Kaptchuk et al. (2022), is well-established, yet the conflation of subjective perception with objective physiological harm remains a clinical pitfall. I strongly recommend integrating objective biomarkers-such as cortisol levels or heart rate variability-alongside self-reporting to mitigate cognitive bias. This approach aligns with the biopsychosocial model endorsed by the WHO.
Steve Harris
November 28, 2025 AT 02:14I’ve been a therapist for 18 years, and this is one of the clearest, most compassionate summaries I’ve seen on this topic. People don’t need more judgment-they need tools and time. The ‘two-week rule’ is gold. I give it to every patient who’s scared. And I tell them: ‘Your body isn’t betraying you. It’s learning.’ Simple. Powerful. Real.
Michael Marrale
November 28, 2025 AT 07:36Okay but have you considered that the FDA is hiding data on long-term brain damage from SSRIs? I know a guy who took Lexapro for 6 months and now he can’t remember his wedding day. And the app you mentioned? SideEffectCope? That’s a Trojan horse. I downloaded it and it asked for my location, my calendar, and my blood pressure readings. Who is behind this? Why do they need all that? I’m not saying you’re evil… but are you *sure* you’re not part of the system?
David vaughan
November 30, 2025 AT 06:59...i just wanted to say thank you. i’ve been on sertraline for 5 months. the first 10 days were hell. i cried every night. i thought i was dying. but i kept the note you mentioned on my lock screen: ‘this happens to 75% of people. it fades by week 3.’ i read it 17 times a day. and… it did fade. i’m not ‘fixed.’ but i’m here. and i’m not alone. ❤️
David Cusack
November 30, 2025 AT 16:30How quaint. You've reduced a complex neuropharmacological phenomenon to a self-help pamphlet. The nocebo effect is a legitimate concept, yes-but to suggest that anxiety alone explains the somatic distress of SSRI withdrawal is to engage in intellectual cowardice. I've reviewed the literature. The data is far messier than your bullet points imply. And frankly, your reliance on Reddit anecdotes as empirical support is… almost endearing in its naiveté.
Elaina Cronin
December 1, 2025 AT 06:46I appreciate the effort put into this article, and I commend the author for addressing such a widespread yet under-discussed issue. However, I must express my deep concern regarding the casual tone used in a context that involves life-altering medical decisions. The phrase ‘take your pill’ is insufficient. Patients require structured follow-ups, clinical monitoring, and empathetic dialogue-not motivational slogans. I urge providers to pair such resources with professional psychiatric oversight.
Willie Doherty
December 1, 2025 AT 11:43As someone who has reviewed over 200 case files involving medication non-adherence, I can confirm that psychological interventions alone are inadequate when access to care is limited. The 32% adherence increase cited? That was in a controlled U.S. trial with subsidized healthcare. In rural India, where patients pay out-of-pocket for pills and have no therapist access, the ‘two-week rule’ is a luxury. We need policy reform, not just mindfulness apps.