Antiplatelet Drug Selector
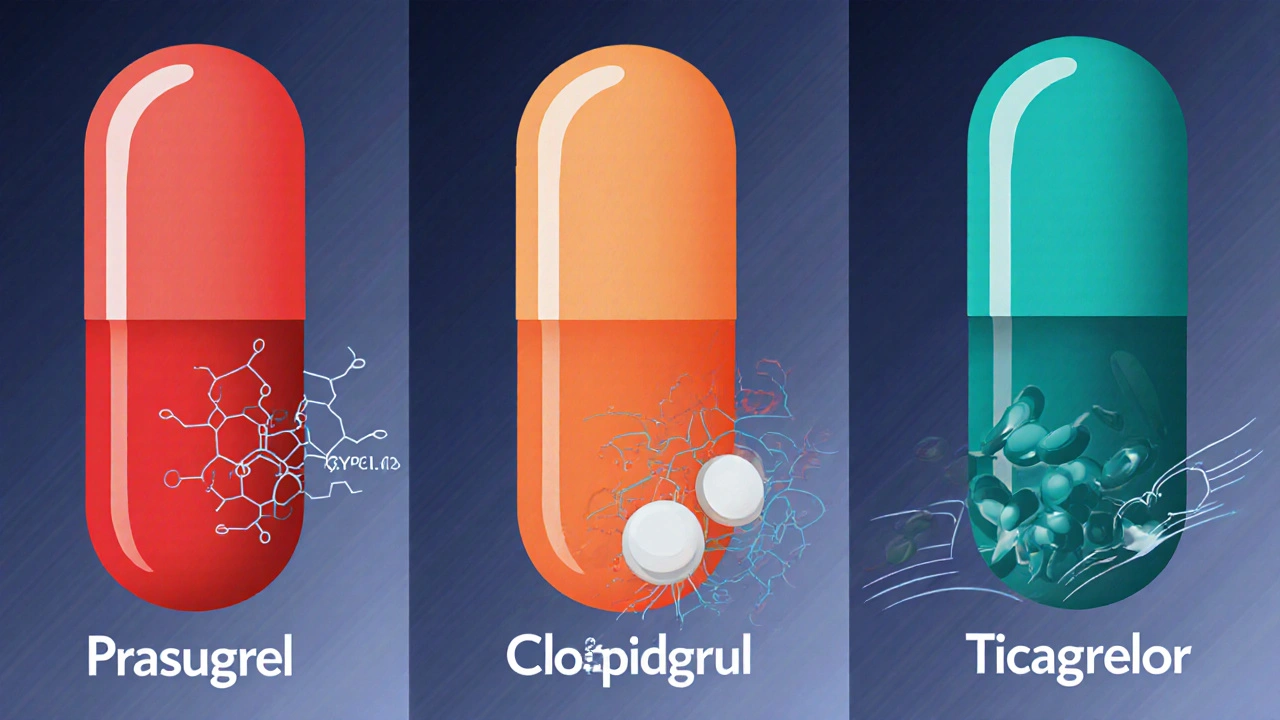
- Prasugrel: Fastest onset, strongest effect - ideal for young, heavy, low-bleed risk patients undergoing PCI.
- Clopidogrel: Cheapest, safer in elderly or low-weight patients - preferred if bleeding risk is high or patient is a poor metabolizer.
- Ticagrelor: Rapid onset, reversible - good for urgent situations or when quick reversal is needed.
When your doctor prescribes a pill to keep a heart attack at bay, the choice isn’t always obvious. Prasugrel has become a popular option, but it sits among several other antiplatelet agents that each have their own strengths and drawbacks. This guide walks you through the key differences so you can see which drug matches your health profile and treatment goals.
What is Prasugrel and how does it work?
Prasugrel is a thienopyridine antiplatelet that irreversibly blocks the P2Y12 receptor on platelets, preventing them from clumping together. After oral ingestion, the pro‑drug is rapidly converted by hepatic enzymes, especially CYP2C19, into its active metabolite. The result is a swift, potent inhibition that peaks in about 30 minutes and lasts for the life of the platelet (7-10 days).
Primary alternatives at a glance
Three other agents dominate the antiplatelet landscape:
- Clopidogrel - also a thienopyridine but slower to activate and more sensitive to genetic variations in CYP2C19.
- Ticagrelor - a cyclopentyltriazolopyrimidine that reversibly binds P2Y12 and does not require metabolic activation.
- Aspirin - an irreversible cyclo‑oxygenase inhibitor that reduces thromboxane A2 production, often used in combination with a P2Y12 blocker as part of dual antiplatelet therapy (DAPT).
How the drugs stack up in clinical trials
Large, randomized studies provide the backbone for decision‑making:
- The TRITON‑TIMI 38 trial showed that Prasugrel reduced the composite endpoint of cardiovascular death, myocardial infarction, or stroke by 2.5% compared with clopidogrel in patients with acute coronary syndrome (ACS) undergoing percutaneous coronary intervention (PCI).
- The PLATO trial demonstrated that Ticagrelor lowered the same endpoint by 1.6% versus clopidogrel, with a quicker onset of action.
- Meta‑analyses suggest that both prasugrel and ticagrelor outperform clopidogrel in high‑risk ACS, but the absolute benefit varies with age, diabetes status, and body weight.
Bleeding risk - the safety trade‑off
All potent antiplatelets increase bleeding, but the magnitude differs:
- Prasugrel carries the highest major bleeding rate (≈2.5% in TRITON‑TIMI 38), especially in patients over 75, weighing less than 60kg, or with a history of stroke.
- Ticagrelor shows a moderate increase (≈2.0% major bleed) but has a reversible effect, allowing faster platelet function recovery after discontinuation.
- Clopidogrel generally yields the lowest bleeding rates, though its efficacy can be compromised in poor metabolizers.
- Aspirin adds a modest bleed risk; when combined in DAPT, the cumulative risk rises, underscoring the need for individualized duration.
Practical considerations for clinicians and patients
Beyond efficacy and safety, real‑world factors shape the prescription decision.
| Drug | Mechanism | Dosing (maintenance) | Onset | Activation | Major trial | Bleeding risk |
|---|---|---|---|---|---|---|
| Prasugrel | Irreversible P2Y12 inhibition | 10mg once daily | ≈30min | CYP2C19‑dependent | TRITON‑TIMI38 | High (↑ in elderly, low weight) |
| Clopidogrel | Irreversible P2Y12 inhibition | 75mg once daily | ≈2h | CYP2C19‑dependent (genetic variability) | CAPRICORN, CURE | Low to moderate |
| Ticagrelor | Reversible P2Y12 inhibition | 90mg twice daily | ≈30sec | Direct‑acting (no metabolism required) | PLATO | Moderate |
| Aspirin | Irreversible COX‑1 inhibition | 81‑325mg once daily | ≈5min | None | Various primary‑prevention trials | Low (gastrointestinal) |
Cost is another decisive factor. In many Australian formularies, clopidogrel is the cheapest option, followed by aspirin. Prasugrel and ticagrelor carry higher out‑of‑pocket expenses, though private insurance may offset the gap for high‑risk patients.
Who should get Prasugrel?
Guidelines from the ACC/AHA recommend prasugrel for patients with ACS undergoing PCI who are:
- Under 75years old
- Weigh more than 60kg
- Without prior stroke or transient ischemic attack
If any of these criteria are violated, clinicians usually switch to clopidogrel or ticagrelor.
Decision matrix - matching drug to patient profile
- Assess bleeding risk: high risk → avoid prasugrel, consider clopidogrel.
- Check CYP2C19 genotype (if available): poor metabolizer → avoid clopidogrel.
- Consider clinical urgency: need rapid platelet inhibition → ticagrelor or prasugrel.
- Evaluate cost and adherence potential: once‑daily dosing (prasugrel, clopidogrel) may improve compliance over twice‑daily ticagrelor.
Plug your answers into the table below to see the best fit.
| Scenario | Preferred drug |
|---|---|
| Young, heavy, ACS + PCI, no bleeding concerns | Prasugrel |
| Elderly (>75) or low body weight | Clopidogrel (or low‑dose aspirin + clopidogrel) |
| Urgent need for rapid effect, can manage twice‑daily dosing | Ticagrelor |
| Known CYP2C19 poor metabolizer | Ticagrelor or prasugrel (if not high‑bleed risk) |
| Low‑cost requirement, moderate risk | Clopidogrel (+ aspirin) |
Quick cheat sheet
- Prasugrel: fastest, most potent, higher bleed - best for young, heavy, low‑bleed patients.
- Clopidogrel: cheaper, safe, but variable efficacy in certain genotypes.
- Ticagrelor: rapid, reversible, moderate cost - good when quick off‑switch may be needed.
- Aspirin: always part of DAPT, low cost, but alone less effective for ACS.
Frequently Asked Questions
What conditions is Prasugrel prescribed for?
Prasugrel is indicated for patients with acute coronary syndrome who undergo percutaneous coronary intervention. It helps prevent clot formation inside stents and reduces heart‑attack recurrence.
How does Prasugrel differ from Clopidogrel?
Both block the same P2Y12 receptor, but Prasugrel activates faster and delivers stronger platelet inhibition. Clopidogrel’s effect relies heavily on the CYP2C19 enzyme, making it less reliable in people with certain genetic variants.
Who should avoid Prasugrel?
Patients over 75years, those weighing under 60kg, or anyone with a prior stroke or transient ischemic attack should not use Prasugrel due to a markedly higher bleeding risk.
Is Ticagrelor reversible?
Yes. Unlike Prasugrel and Clopidogrel, Ticagrelor binds reversibly, allowing platelet function to recover within a few days after stopping the drug.
Can I take Aspirin with Prasugrel?
Aspirin is typically combined with a P2Y12 blocker as part of dual antiplatelet therapy. For most ACS patients, a low‑dose aspirin (75‑81mg) alongside Prasugrel is standard practice, unless contraindicated for gastrointestinal bleeding.

Ryan Hlavaty
October 5, 2025 AT 01:36Prescribing the strongest antiplatelet for every patient is a moral failing; we must prioritize safety over blind efficacy. Young, heavy patients may tolerate prasugrel, but the elderly and those with bleeding risk deserve the gentler clopidogrel. Ignoring these guidelines is reckless and endangers lives. Doctors should act with compassion, not with a reckless appetite for the newest drug. The stakes are too high for careless shortcuts.
Chris Faber
October 7, 2025 AT 09:09hey folks just wanted to say i think the guide does a good job of breaking things down friendly style cheers
aura green
October 9, 2025 AT 16:42Wow, the world of antiplatelets is a roller‑coaster of science, economics, and pure drama 😅
First off, the difference between prasugrel and clopidogrel is not just a fancy marketing gimmick, it’s about how fast and how hard the platelet blockade hits.
Prasugrel is like a sprinter – it bursts onto the scene with a 30‑minute onset, ideal for those urgent PCI cases where every second counts.
Clopidogrel, on the other hand, prefers to take a leisurely stroll, taking about two hours to get into gear, which can be problematic for high‑risk patients.
But wait, genetics love to throw a wrench in the works: CYP2C19 poor metabolizers can turn clopidogrel into a placebo, leaving patients unprotected.
This is where ticagrelor shines, because it doesn’t need that enzymatic activation, making it a reliable choice for genetically diverse populations.
Now, let’s talk bleeding – the holy grail of safety. Prasugrel’s potency comes with a price, especially in patients over 75 or under 60 kg, where major hemorrhage rates climb like a scary horror movie.
Clopidogrel generally keeps the bleeding risk in check but may sacrifice some efficacy, especially in those unlucky genetic profiles.
Ticagrelor offers a middle ground: strong, rapid, and reversible – you can pull the plug quicker if bleeding becomes an issue.
Cost is the sneaky villain in this saga; clopidogrel is cheap, while prasugrel and ticagrelor can burn a hole in your wallet unless insurance steps in.
Guidelines from the ACC/AHA give us a roadmap: young, heavy, low‑bleed‑risk patients undergoing PCI can safely ride the prasugrel express, whereas older or lighter patients should stick to clopidogrel or maybe ticagrelor if you need speed.
In the end, the best drug is the one that matches the patient’s age, weight, genetic makeup, bleeding risk, and budget – not the one that sounds the coolest.
So, next time your cardiologist reaches for a pill, ask the right questions and remember: science, not hype, should drive the decision. 😊
Edward Morrow
October 11, 2025 AT 10:22Listen up, this isn’t some overpriced gimmick – if you’re not using the right drug you’re basically shooting yourself in the foot, plain and simple.
Shayne Tremblay
October 13, 2025 AT 12:22Great points! Remember to keep the conversation patient‑centered. If you’re unsure about genetic testing, discuss options with your cardiologist and weigh the benefits of each drug. Staying proactive can make a huge difference in outcomes.
Stephen Richter
October 14, 2025 AT 21:42Indeed, a thorough risk assessment is essential. One should also consider the duration of dual antiplatelet therapy and individual tolerance when selecting an agent.
Musa Bwanali
October 17, 2025 AT 05:16Let’s keep it practical: for most ACS patients undergoing PCI, I’d start with prasugrel if they’re under 75 and over 60 kg, otherwise fall back to clopidogrel. Ticagrelor is perfect when you need a rapid reversible effect, like before surgery. This framework keeps you safe and effective.
Allison Sprague
October 18, 2025 AT 17:22While your "practical" flowchart sounds convenient, it dangerously oversimplifies complex pharmacogenomics. Many clinicians still prescribe clopidogrel without testing, leading to suboptimal inhibition in poor metabolizers. Such blanket statements can mislead readers into complacency.
leo calzoni
October 20, 2025 AT 19:22Honestly, the whole debate is a distraction from the fact that most of these trials are industry‑sponsored, and the data is cherry‑picked to favor newer, more expensive agents. A simple, inexpensive clopidogrel regimen remains clinically sound for the majority.
KaCee Weber
October 22, 2025 AT 13:02Interesting take! 🌟 While industry influence is a real concern, we can’t ignore that newer agents have shown statistically significant reductions in composite endpoints for certain high‑risk populations. It’s about balancing cost with clinical benefit, not dismissing innovation outright. 😊
jess belcher
October 24, 2025 AT 20:36Both perspectives have merit; cost considerations are real, yet outcomes matter most. It’s essential to personalize therapy based on patient specifics.
Sriram K
October 26, 2025 AT 07:42Absolutely. If you have access to CYP2C19 testing, it can guide you away from clopidogrel when needed. Otherwise, ticagrelor provides a reliable alternative without metabolic concerns.
Deborah Summerfelt
October 28, 2025 AT 09:42But what if the whole premise of “personalized” therapy is just a buzzword? The average patient probably won’t benefit from all this nuance.
Taryn Bader
October 30, 2025 AT 03:22I can’t believe anyone would even suggest that!
Myra Aguirre
November 1, 2025 AT 10:56It’s good to see a calm discussion. Let’s keep the focus on what works best for patients without getting too heated.
Shawn Towner
November 2, 2025 AT 23:02While calmness is admirable, we must also challenge the status quo and ask why we accept these guidelines without questioning their origins.
Ujjwal prakash
November 5, 2025 AT 01:02Honestly, the data is crystal clear-prasugrel is superior in low‑bleed‑risk patients!!! However, when you throw in age>75, weight<60kg, and prior stroke, the risk skyrockets!!! So, you have to balance the super‑strong platelet inhibition against the bleeding catastrophe!!! This isn’t a one‑size‑fits‑all scenario; it’s a delicate calculus!!!
Diane Helene Lalande
November 6, 2025 AT 18:42Exactly, the risk‑benefit ratio must guide our choice. Encouraging patients to discuss these factors with their providers can lead to better outcomes.
Edwin Levita
November 9, 2025 AT 02:16All this talk about ratios and risks makes me feel like I’m reading a soap opera-so much drama over a tiny pill! Yet, I get it; the stakes are real.