Photosensitivity Medication Risk Checker
Check Your Medication Risk
Identify medications that increase your risk of photosensitivity and get personalized sun safety recommendations
Did you know that some of the most common medications you take - like antibiotics, blood pressure pills, or even ibuprofen - can turn a normal day outside into a painful sunburn? It’s not just about getting too much sun. It’s about what’s in your body reacting to it. This isn’t rare. Around 8-20% of people on certain medications experience this. And most don’t even know they’re at risk until their skin starts burning through clothes or blistering after a short walk.
What Exactly Is Medication-Induced Photosensitivity?
Photosensitivity from medications happens when a drug in your system reacts with ultraviolet (UV) light - mostly UVA rays - and triggers a skin reaction. It’s not an allergy in the traditional sense. It’s a chemical reaction. Think of it like your skin suddenly becoming extra sensitive to sunlight because of something you swallowed or applied. There are two main types: phototoxic and photoallergic. Phototoxic is the big one - making up about 95% of cases. It’s like an exaggerated sunburn. You get redness, swelling, stinging, and sometimes blisters - all within minutes to a couple of hours after sun exposure. It only happens where the sun hits your skin. If you took doxycycline for acne and walked outside without sunscreen, you could burn badly even through a T-shirt. Photoallergic is rarer - only about 5% - but trickier. It acts like a delayed allergic rash. You might not notice anything for a day or two. Then, it shows up as an itchy, patchy rash that can spread beyond sun-exposed areas. This one can happen even if you’ve taken the same drug before without issue. The key difference? Phototoxic = immediate, dose-dependent, everyone can get it. Photoallergic = delayed, immune-driven, only some people.Which Medications Cause the Most Problems?
You might be surprised. It’s not just the obvious ones. Here are the usual suspects:- Tetracycline antibiotics - Doxycycline causes reactions in 10-20% of users. It’s one of the most common causes.
- NSAIDs - Ketoprofen (found in some pain creams) and even ibuprofen can trigger reactions in a small but real number of people.
- Fluoroquinolones - Ciprofloxacin and levofloxacin are linked to phototoxic burns, especially in older adults.
- Amiodarone - A heart medication used for irregular rhythms. Up to 75% of long-term users develop lasting photosensitivity. Some people still react years after stopping it.
- Sulfonamides - Antibiotics like Bactrim. Often linked to photoallergic rashes.
- Diuretics - Hydrochlorothiazide, commonly prescribed for high blood pressure, is a known trigger.
- Some antidepressants and acne treatments - Retinoids like isotretinoin and certain SSRIs can increase sensitivity.
And here’s something most people don’t realize: 40% of photosensitivity cases come from antibiotics. Another 25% come from heart and blood pressure meds. If you’re on any of these, you’re not just at risk - you’re in a high-risk group.
Why Regular Sunscreen Often Fails
Most people think SPF 30 or 50 is enough. It’s not. The problem isn’t just the number. It’s what’s in the product. Many sunscreens block UVB rays (the ones that cause sunburn) really well. But they don’t do enough against UVA - the longer wavelengths that penetrate deeper and trigger photosensitivity reactions. The FDA says only 35% of SPF 50+ sunscreens actually offer enough UVA protection based on critical wavelength testing. So what works? Look for these ingredients:- Zinc oxide - At least 15% concentration. It physically blocks both UVA and UVB.
- Titanium dioxide - Also a physical blocker. Works well with zinc.
Avoid chemical filters like oxybenzone and octinoxate - they’re common in sunscreens, but they can themselves be photoallergens. That’s right: the sunscreen you’re using might be part of the problem.
And here’s the catch: most people apply only 25-50% of the amount needed. To get full protection, you need about 1 ounce - a shot glass full - for your whole body. Reapply every two hours, or after sweating or swimming. If you’re on a high-risk medication, treat sunscreen like medicine: non-negotiable, timed, measured.
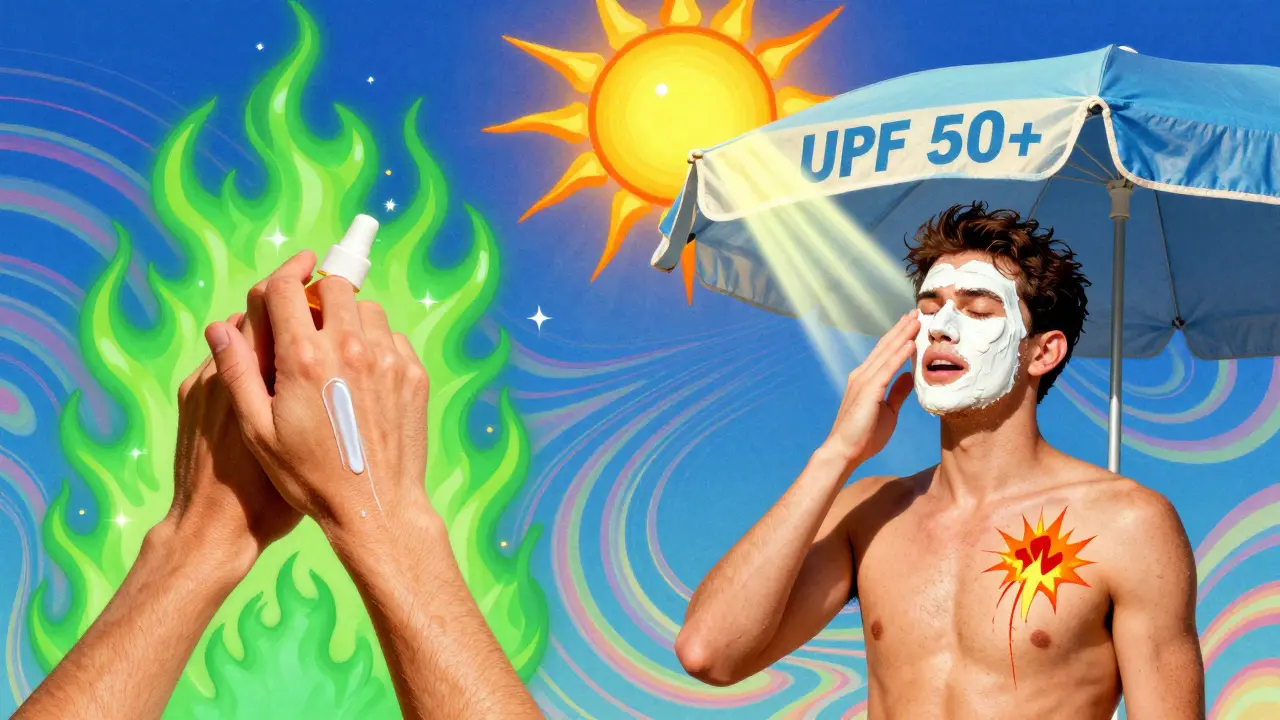
Clothing Is Your Best Defense
A T-shirt gives you maybe 3-20% UV protection. That’s barely better than nothing. But UPF 50+ clothing? That blocks 98% of UV rays. Brands like Solbari, Coolibar, and UV Skinz make shirts, hats, and even swimwear designed for people with photosensitivity. People who switch to UPF 50+ clothing report 90% fewer reactions. One user on a patient forum said, “I used to get burned walking to my car. Now I wear my UPF shirt, walk outside at noon, and feel nothing.” Don’t just rely on color or thickness. Look for the UPF label. A dark, tightly woven shirt might look protective, but unless it’s tested and labeled UPF 50+, it’s not reliable. And hats? Wide-brimmed ones (over 3 inches) are better than baseball caps. Your ears, neck, and scalp are common sites for reactions.What No One Tells You About Timing and UV Index
It’s not just about being outside. It’s about when and how much UV is in the air. The UV index isn’t just for beach days. Even on cloudy days in Sydney, the UV index can hit 8 or 9 in January. And it’s rising - 0.5-1.0% per year due to climate change. That means more risk, more often. Use an app like UVLens or the SunSmart app (free, from the Australian Cancer Council). They give you real-time UV levels. If the index is above 3, you’re at risk. That’s not just summer. That’s spring, fall, even winter in Australia. Plan your outdoor time before 10 a.m. or after 4 p.m. When the sun is highest, stay indoors if you can. Even brief exposure - like walking to the mailbox or waiting for the bus - can trigger a reaction if you’re on the wrong medication.Why Doctors Often Miss This
Here’s the uncomfortable truth: most doctors don’t warn you. A survey of 1,200 patients found that 68% received no sun safety advice when they were prescribed a photosensitizing drug. Dermatologists know. Primary care doctors? Not so much. Only 35% of primary care practices screen for photosensitivity risk. Meanwhile, dermatology clinics have been doing it for years. If you’re prescribed a new medication - especially antibiotics, heart meds, or diuretics - ask: “Can this make me more sensitive to the sun?” Don’t wait for a reaction. Ask before you start. And if you’ve had an unexplained sunburn or rash after being in the sun, bring up photosensitivity. Many cases get misdiagnosed as “polymorphic light eruption” or “idiopathic sun sensitivity.” But if it’s drug-related, you need different advice - not just “use more sunscreen.”
What’s New in 2026
There’s real progress. In 2023, the FDA approved the first targeted photoprotective medication - Lumitrex (photoprotectin). It doesn’t replace sunscreen, but it reduces UV-induced skin damage by 70% in clinical trials. It’s still new, but it’s a sign that the medical world is finally taking this seriously. Genetic testing is also entering the picture. Companies like 23andMe now offer a photosensitivity risk panel that checks for gene variants linked to higher reaction risk. If you’ve had bad sun reactions before, even without meds, this test might help you understand why. And the clothing market? It’s growing fast. The global photoprotective clothing industry hit $3.2 billion in 2022, and it’s still rising. More people are demanding real protection - not just marketing.What You Can Do Today
If you’re on medication and spend time outdoors, here’s your action plan:- Check your meds - Look up your prescription on the FDA’s Sun Safety Medication Database or ask your pharmacist.
- Ask your doctor - “Is this drug linked to sun sensitivity? What should I do?”
- Use zinc oxide sunscreen - SPF 50+, 15%+ zinc oxide, reapplied every 2 hours.
- Wear UPF 50+ clothing - Hats, long sleeves, UV-blocking sunglasses.
- Monitor the UV index - Avoid being outside when it’s above 3.
- Track your reactions - Keep a simple log: date, meds taken, sun exposure, symptoms. It helps your doctor.
This isn’t about being paranoid. It’s about being informed. Photosensitivity isn’t just a rash. It can lead to chronic skin damage - and even increase your risk of skin cancer by up to 60% over time. You don’t have to stop living outside. You just need to protect yourself the right way.
When to See a Dermatologist
If you’ve had:- Blistering or peeling skin after sun exposure while on medication
- A rash that spreads beyond sun-exposed areas
- Dark patches or discoloration that won’t fade
- Repeated reactions despite using sunscreen and clothing
It’s time to see a dermatologist. They can do a photopatch test to confirm if it’s photoallergic. They can also help you find safer alternatives to your current meds if possible.
And if you’re a caregiver - for an elderly parent, for example - make sure they’re protected. Many older adults take multiple photosensitizing drugs. They’re often unaware of the risk. A simple conversation could prevent a trip to the ER.
Can I still go outside if I’m on a photosensitizing medication?
Yes, but you need to be smarter about it. Avoid direct sun between 10 a.m. and 4 p.m. Wear UPF 50+ clothing, use zinc oxide sunscreen, and check the UV index daily. You don’t have to stay indoors - just protect yourself like you would in a high-risk environment.
Do I need to stop my medication if I get a sun reaction?
Never stop a prescribed medication without talking to your doctor. Many reactions can be managed with better sun protection. But if the reaction is severe or recurring, your doctor may switch you to a different drug. For example, switching from doxycycline to another antibiotic often eliminates the problem.
Is this only a problem in summer?
No. UVA rays are present year-round and penetrate clouds and glass. You can get a reaction in winter, on cloudy days, or even through a window. That’s why daily protection matters - not just beach days.
Can I use tanning beds if I’m on these meds?
Absolutely not. Tanning beds emit intense UVA radiation - the exact type that triggers phototoxic reactions. Using them while on photosensitizing drugs can cause severe burns, blistering, and long-term skin damage. It’s a high-risk activity you should avoid entirely.
Are natural or organic sunscreens safe?
Not necessarily. Many “natural” sunscreens lack sufficient UVA protection. Look for zinc oxide or titanium dioxide as the active ingredients - not just “natural” or “organic” on the label. If it doesn’t say SPF 50+ and list zinc oxide at 15% or higher, it’s not reliable for medication-induced photosensitivity.
Will my skin return to normal after stopping the medication?
For phototoxic reactions, yes - usually within weeks or months after stopping the drug. But for some medications like amiodarone, sensitivity can last for years. Photoallergic reactions may resolve faster, but the skin can remain sensitive. Always continue sun protection until your doctor says it’s safe to ease up.

matthew martin
January 28, 2026 AT 02:38Whoa. I’ve been on doxycycline for years and thought I was just ‘bad at sunscreen.’ Turns out I was basically walking around with a UV sponge. This post just saved my skin - and maybe my future self from looking like a raisin. UPF shirts? I’m buying three. No more guessing.
Mindee Coulter
January 28, 2026 AT 08:11My grandma’s on amiodarone and got burned through her blouse last summer. I’m printing this out for her doctor. Thank you.
Linda O'neil
January 29, 2026 AT 16:50I used to think sunscreen was just for beach days. Now I slap on zinc oxide before walking the dog at 7 a.m. I don’t care how it looks - I’d rather be pale and unburnt than red and in pain. This is life-changing info.
Colin Pierce
January 30, 2026 AT 16:47Just checked my meds - hydrochlorothiazide. Oh. So that’s why my shoulders look like they survived a campfire. I’ve been using that ‘natural’ sunscreen with coconut oil and thinking I was being healthy. Nope. Time to upgrade. Thanks for the clarity.
Chris Urdilas
January 30, 2026 AT 23:37They say ‘sun safety’ like it’s a lifestyle choice. Nah. It’s a damn medical necessity if you’re on half the prescriptions floating around. I’ve seen people in their 70s with skin like cracked leather because no one told them. This isn’t hype - it’s harm reduction. Pass it on.
Katie Mccreary
February 1, 2026 AT 17:14So now we’re blaming the meds AND the sunscreen? What’s next? The sun is a government tool? 😏
Lexi Karuzis
February 2, 2026 AT 17:05They don’t warn you because they don’t want you to know that Big Pharma profits more from treating skin cancer than from preventing it. They know you’ll keep taking the pills and just buy more sunscreen. And more expensive UPF clothes. And more dermatologist visits. And then… they’ll patent the next ‘miracle’ cream. It’s a loop. A very profitable loop.
Phil Davis
February 4, 2026 AT 07:49So… I’m supposed to wear a spacesuit to the mailbox now? Cool. I’ll just stay inside until 2050. Or maybe I’ll start a support group: ‘People Who Got Burned by Their Own Prescriptions.’ We’ll meet under fluorescent lighting. No windows allowed.
Jeffrey Carroll
February 5, 2026 AT 10:45While the information presented is clinically accurate and well-sourced, I would respectfully suggest that the tone, though engaging, may unintentionally amplify anxiety among patients. A more balanced approach - emphasizing risk mitigation rather than alarm - might better serve the broader audience. That said, the data on UVA penetration and UPF efficacy is unequivocally valuable.
Rhiannon Bosse
February 7, 2026 AT 00:18Okay but have you seen the price of UPF 50+ swimwear?? $120 for a shirt?? And they charge extra for the hat?? I’m not paying that for fabric. I’ll just stay inside. Or wear a hoodie. And cry. 😭
Brittany Fiddes
February 8, 2026 AT 13:35Interesting. In the UK, we’ve had public health campaigns about this since 2015. Here in the US, it’s like everyone’s still living in 2003. You’d think with all the melanoma stats, someone would’ve made a PSA by now. But no. We’d rather watch influencers tan on TikTok. Pathetic.
Robert Cardoso
February 9, 2026 AT 11:34Photosensitivity isn’t a medical condition - it’s a philosophical one. It forces us to confront our relationship with sunlight, with chemical dependency, with the illusion of control. We take pills to fix ourselves, then blame the sun when our bodies rebel. But the sun doesn’t care. It just is. The real question: Are we willing to change our habits - or just keep buying more sunscreen?
Amber Daugs
February 10, 2026 AT 00:21Ugh. I knew someone who got a rash from ibuprofen and now she’s obsessed with ‘detoxing’ and drinking lemon water at 5 a.m. It’s not a detox. It’s a drug reaction. Stop making it spiritual. Just wear the shirt. Use the zinc. End of story.
SRI GUNTORO
February 11, 2026 AT 21:37My mother in India takes blood pressure medicine and never wears sunscreen. She says, ‘Sun is God’s gift.’ But now I send her UPF shirts from Amazon. She wears them grudgingly. Still, she hasn’t burned in 8 months. Maybe tradition needs updating.
Mark Alan
February 12, 2026 AT 23:17🚨 I JUST REALIZED I’M ON TWO OF THESE DRUGS. 🚨 I’M WEARING A HAT AND A COAT TO THE GROCERY STORE TOMORROW. 🌞🔥 #SunSafetyIsNotAClimateIssue #ZincOxideIsMySavior