When you’re in severe pain, opioids can feel like a lifeline. But for many people, what starts as short-term relief turns into something far more dangerous. Opioid therapy isn’t a one-size-fits-all solution - and using it the wrong way can lead to dependence, overdose, or even death. The key isn’t avoiding opioids entirely, but knowing when they’re truly needed - and when they’re not.
When Opioids Might Actually Help
Opioids aren’t evil drugs. They’re powerful tools that, when used correctly, can make a real difference. The CDC and other major medical groups agree: opioids are appropriate for severe acute pain - like after major surgery, a broken bone, or serious trauma. In these cases, they’re often the most effective option for getting someone through the first few days or weeks. But here’s where most mistakes happen: opioids are rarely the right first choice for long-term pain. If you’ve had back pain for six months, or arthritis that’s been flaring for years, guidelines from the CDC, VA, and Kaiser Permanente all say: try everything else first. Physical therapy, NSAIDs like ibuprofen, nerve blocks, acupuncture, or even cognitive behavioral therapy are safer, often just as effective, and don’t carry the risk of addiction. The bottom line? Opioids should be a last resort for chronic pain - not the default. If your doctor suggests them right away, ask: What else have we tried? If the answer is nothing, that’s a red flag.How Much Is Too Much?
Dose matters - a lot. The CDC says that for most people, staying under 50 morphine milligram equivalents (MME) per day keeps overdose risk low. But once you cross 90 MME, your risk of overdose jumps dramatically. At 100 MME or more, about 1 in 4 people develop opioid use disorder. What does that look like in real life? A typical prescription for oxycodone 5mg, taken four times a day, equals 20 MME. Add a hydrocodone 10mg once a day, and you’re at 30 MME. That’s still within the safer range. But if you’re on 12 oxycodone 10mg pills a day? That’s 120 MME - well into danger territory. Doctors aren’t supposed to push doses this high without a clear reason and extra safeguards. If you’re on high-dose opioids and haven’t had a serious review of your treatment plan in the last 90 days, it’s time to ask questions.The Hidden Dangers: Mixing Drugs
One of the most dangerous - and often overlooked - risks isn’t the opioid itself, but what it’s mixed with. Benzodiazepines, like Xanax or Valium, are commonly prescribed for anxiety or sleep. But when taken with opioids, they can slow your breathing to a stop. The CDC found that people who take both have nearly four times the risk of overdose compared to those on opioids alone. Other risky combinations include alcohol, sleep aids, muscle relaxants, and even some antidepressants. If you’re on opioids, your pharmacist should flag these interactions. If they don’t, ask. Keep a full list of everything you take - including supplements and over-the-counter meds - and bring it to every appointment.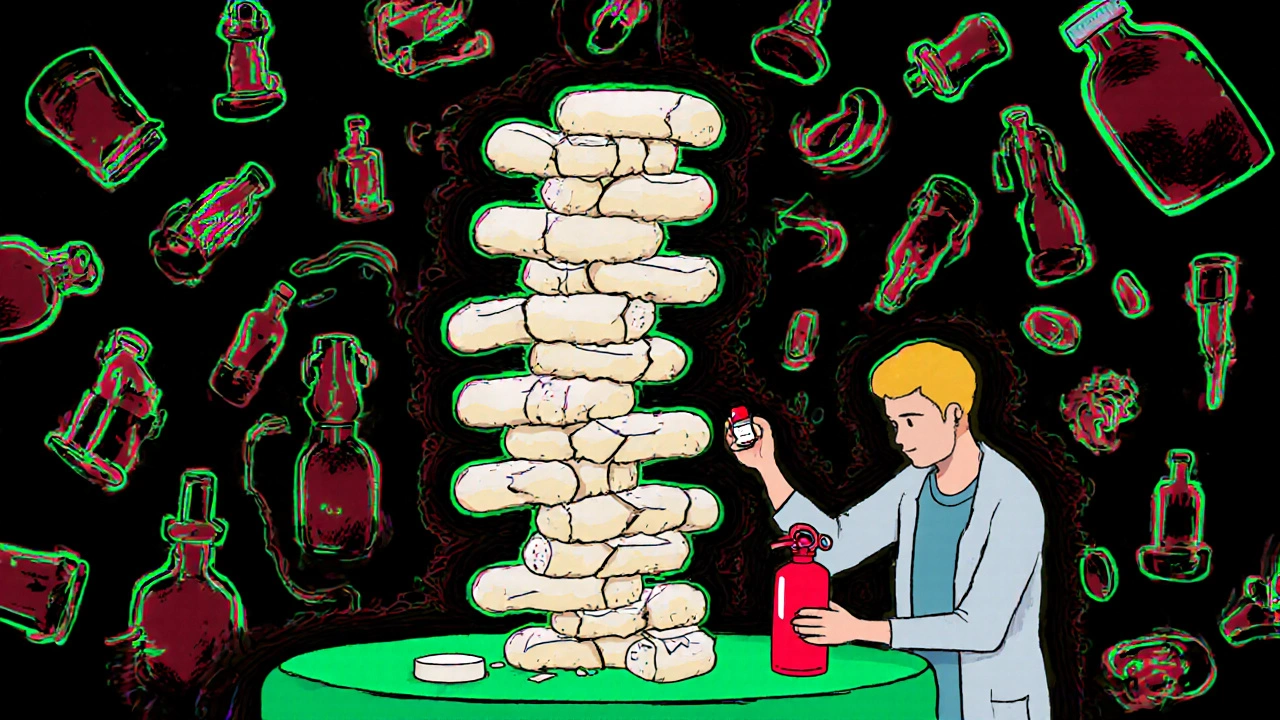
Who’s at Highest Risk?
Not everyone who takes opioids becomes dependent. But some people are far more vulnerable. Risk factors include:- A personal or family history of substance use disorder
- Being over 65 (older bodies process drugs slower)
- Having untreated depression or anxiety
- Using opioids for more than 90 days without clear improvement
Monitoring and Tapering: What Good Care Looks Like
Good opioid care isn’t just about writing a prescription. It’s about ongoing check-ins. The CDC and VA recommend regular reviews - at least every three months for stable patients, and monthly if you’re high-risk. These visits should include:- Measuring your pain on a scale of 0-10
- Assessing your ability to do daily tasks - walking, sleeping, working
- Urine drug tests to confirm you’re taking what’s prescribed
- Screening for signs of misuse using tools like the Current Opioid Misuse Measure
The Bigger Picture: Why Prescriptions Are Falling
In 2012, doctors in the U.S. wrote 81 prescriptions for every 100 people. By 2020, that number dropped to 47. That’s not because pain disappeared - it’s because doctors learned better. Prescription Drug Monitoring Programs (PDMPs) are now used in 49 states. Before writing an opioid script, doctors can check if you’re getting pills from other providers. Most hospitals now have standing orders for naloxone. And the NIH is pouring $1.5 billion a year into developing non-addictive pain treatments - 37 of which are already in late-stage trials. But progress isn’t perfect. A 2021 study found that only 37% of primary care doctors consistently use risk assessment tools. Nearly 70% of ER doctors say they don’t have enough time to do proper evaluations. And in many places, there’s still no clear path to get someone into addiction treatment if they need it.
What You Can Do
If you’re on opioids:- Ask your doctor: “Is this still helping me function better?”
- Request a naloxone prescription if you’re on 50+ MME or take benzodiazepines.
- Never share your pills - even with family members in pain.
- Dispose of unused pills safely - most pharmacies offer take-back programs.
- Track your pain and function weekly. If it’s not improving, bring it up.
- Dependence isn’t failure. It’s a biological response to long-term use.
- Medication-assisted treatment (MAT) with buprenorphine or methadone is the most effective way to manage opioid use disorder.
- You don’t have to quit cold turkey. Support is available.
Frequently Asked Questions
Are opioids ever safe for long-term pain?
Yes - but only in rare cases. For most people with chronic pain, opioids offer little long-term benefit and carry high risks. They may be considered if all other treatments have failed, and only if the patient shows clear improvement in pain and function without side effects. Even then, doses should stay under 50 MME per day, and regular monitoring is required.
Can I get addicted if I take opioids exactly as prescribed?
Yes - addiction isn’t about how you take them, it’s about how your brain responds. About 8-12% of people on long-term opioids develop opioid use disorder, even when following their doctor’s instructions. Genetic factors play a big role, and some people are simply more vulnerable. That’s why risk screening and monitoring are so important.
What should I do if my doctor wants to stop my opioids suddenly?
Refuse. Abruptly stopping opioids can cause severe withdrawal, panic, and even increase the risk of relapse to illegal drugs. The CDC and American Medical Association both warn against rapid tapers. Ask for a slow, personalized plan - usually 5-10% reduction every 4-8 weeks. If your doctor won’t help, seek a pain specialist or addiction medicine provider.
Is it true that opioids don’t work well for chronic pain over time?
Yes. Studies show opioids may reduce pain by only 0.6 to 1.8 points on a 10-point scale in the first few weeks - and that benefit fades after a few months. Meanwhile, risks like tolerance, dependence, and side effects keep growing. For long-term pain, non-opioid treatments like exercise, therapy, and nerve-targeted meds often work better and last longer.
How do I know if I’m developing dependence?
Signs include needing higher doses for the same relief, feeling anxious or irritable when the pill wears off, craving the medication, or using it to cope with stress - not just pain. If you’re taking more than prescribed, hiding use, or skipping activities because of side effects, it’s time to talk to your doctor or a specialist.
Can I switch to non-opioid treatments after being on opioids for years?
Absolutely. Many people do - and feel better. A slow taper, combined with physical therapy, cognitive behavioral therapy, or nerve blocks, often leads to improved function and less reliance on meds. It’s not easy, but it’s possible. Support groups and pain clinics specializing in tapering can help you through it.

Victoria Short
November 16, 2025 AT 19:29My grandma was on oxycodone for 7 years after a fall. She didn't get addicted, but she couldn't walk without it. Doctors just kept prescribing. No PT, no nothing. Now she's on methadone and says she feels more like herself than she has in a decade. Just saying.
Eric Gregorich
November 18, 2025 AT 08:41Let’s be real here - the opioid crisis wasn’t created by patients. It was engineered by pharmaceutical execs who bribed doctors, rewrote guidelines, and turned pain into a profit center. We’re now punishing the very people who trusted the system. The real villain isn’t the woman on 80 MME trying to get out of bed - it’s the $12 billion marketing budget that told her it was safe. And now we’re gaslighting her into feeling guilty for surviving? That’s not harm reduction. That’s moral cowardice dressed up as public health.
Koltin Hammer
November 19, 2025 AT 10:21I’ve seen this play out in rural Appalachia and in Silicon Valley alike. The difference? One side gets compassion. The other gets labeled ‘drug-seeking.’ Opioids don’t discriminate - but the system sure does. I’ve got a cousin in Ohio on buprenorphine who works two jobs and coaches his kid’s soccer team. Meanwhile, my friend in LA got cut off cold turkey and ended up on heroin because no one offered her a taper or a therapist. It’s not about the drug. It’s about who gets to be seen as human.
Phil Best
November 20, 2025 AT 17:18Oh wow, a 12-page medical pamphlet with footnotes. Did you also include the FDA’s 2019 warning about ‘unapproved opioid formulations’? Because I didn’t see that. 😏 Let me guess - your doctor’s office has a laminated copy of the CDC guidelines taped to the fridge next to the ‘No Smoking’ sign. Meanwhile, I’ve got a friend who’s been on 150 MME for 14 years after a car crash - and he’s the most functional person I know. Maybe the guidelines don’t know everything. Just saying.
Parv Trivedi
November 22, 2025 AT 11:31As someone from India, where pain management is often ignored due to stigma or lack of access, I’m glad to see this discussion. But I also worry - in places like mine, even basic NSAIDs are hard to get. So while we talk about tapering in the US, many are still suffering without any relief. Balance matters. Compassion matters more.
Willie Randle
November 23, 2025 AT 17:30Let’s clarify terminology: dependence is not addiction. Dependence is physiological adaptation. Addiction is compulsive use despite harm. These are not interchangeable. When clinicians conflate them, they mismanage care. This post correctly distinguishes them - and that’s rare. Thank you.
Connor Moizer
November 24, 2025 AT 08:15You think you’re helping by scaring people off opioids? Nah. You’re just making people afraid to ask for help. I’ve seen people go from 60 MME to zero in 3 weeks. They cried in the ER. One guy OD’d on fentanyl because he couldn’t get his script. You don’t fix a crisis by abandoning the people in it. You fix it by giving them tools - not guilt trips.
kanishetti anusha
November 26, 2025 AT 00:20My aunt was prescribed opioids after spine surgery. She tracked her pain daily, went to PT, and asked for naloxone. She tapered over 8 months. Now she hikes. She didn’t need to be punished - she needed guidance. This post gets it. Thank you.
roy bradfield
November 27, 2025 AT 13:07Did you know the CDC guidelines were written by a guy who used to work for Purdue Pharma? And the ‘50 MME’ limit? It was pulled out of thin air after a 2016 meeting with no patient input. The whole thing’s a corporate cover-up. They want you scared. They want you off opioids so they can sell you their $12,000 spinal stimulator. Wake up.
Patrick Merk
November 27, 2025 AT 22:10Love this. In Ireland, we’ve got a quiet but growing movement around harm reduction - pharmacies handing out naloxone like candy, GPs trained in MAT, and zero judgment. It’s not perfect, but it’s human. The US could learn a lot from how we handle this without the drama.
Liam Dunne
November 29, 2025 AT 01:27My brother’s a pain specialist. He says the biggest mistake? Assuming everyone’s the same. One person’s miracle drug is another’s nightmare. That’s why personalized care - not one-size-fits-all rules - is the only way forward. Guidelines are starting points, not scripture.
Vera Wayne
November 29, 2025 AT 06:59I’ve been on 40 MME for 3 years. I don’t feel high. I feel functional. I work. I parent. I garden. I’m not ‘addicted.’ I’m managing. And yes - I’ve had my dose reduced twice because of ‘guidelines.’ Both times, my pain spiked. My quality of life cratered. Please stop telling people what their bodies need.
Rodney Keats
November 29, 2025 AT 20:45Oh wow, the CDC is the new Bible now? Next you’ll be telling me to wear sunscreen and eat kale. I’m on 110 MME. I’ve got a PhD. I’ve read the studies. You think I don’t know the risks? I’m still here. And I’m not dying. So maybe, just maybe, the math isn’t as simple as you think.
Laura-Jade Vaughan
November 30, 2025 AT 09:16OMG this is SO important!! 🙌 I’ve been on opioids since 2018 and I’m basically a superhero now. I just started doing yoga and I’m crying happy tears 💖💖💖 also, my therapist says I’m ‘in recovery’ but I don’t feel sick? Like… is that even possible?? 🤔
Jennifer Stephenson
December 1, 2025 AT 00:52Appropriate use of opioids is supported by evidence. Inappropriate use is not. The distinction is critical.
Segun Kareem
December 1, 2025 AT 15:37In Nigeria, pain is often ignored because we don’t have the resources. But I’ve seen people take tramadol like candy because it’s cheap and available. No one monitors them. No one cares. This conversation needs to be global - not just American.
Philip Rindom
December 2, 2025 AT 10:49My uncle got cut off cold turkey last year. He died by suicide six months later. The system didn’t fail him because he used opioids. It failed him because no one offered him a way out - just a wall.
Jess Redfearn
December 4, 2025 AT 03:26Wait so if I’m on 90 MME and I don’t have a family history of addiction, am I fine? Or do I need a therapist, a urine test, a letter from my priest, and a signed waiver from my dog?
Ashley B
December 4, 2025 AT 13:56They’re lying. They’re all lying. The DEA, the CDC, the AMA - they’re just trying to control us. You think they care about your pain? No. They care about control. They want you docile. They want you quiet. Don’t let them take your pills. Don’t let them take your life.
Rebekah Kryger
December 5, 2025 AT 18:03My doctor told me to taper. I asked why. He said ‘because you’re on 70 MME.’ I said ‘but I’m functional.’ He said ‘it’s not about function, it’s about risk.’ I walked out. I’m not a statistic.