Shift Worker Medication Safety Checker
Check Your Medication Safety
Enter your medication details to get safety recommendations based on FDA guidelines and shift work research.
Medications
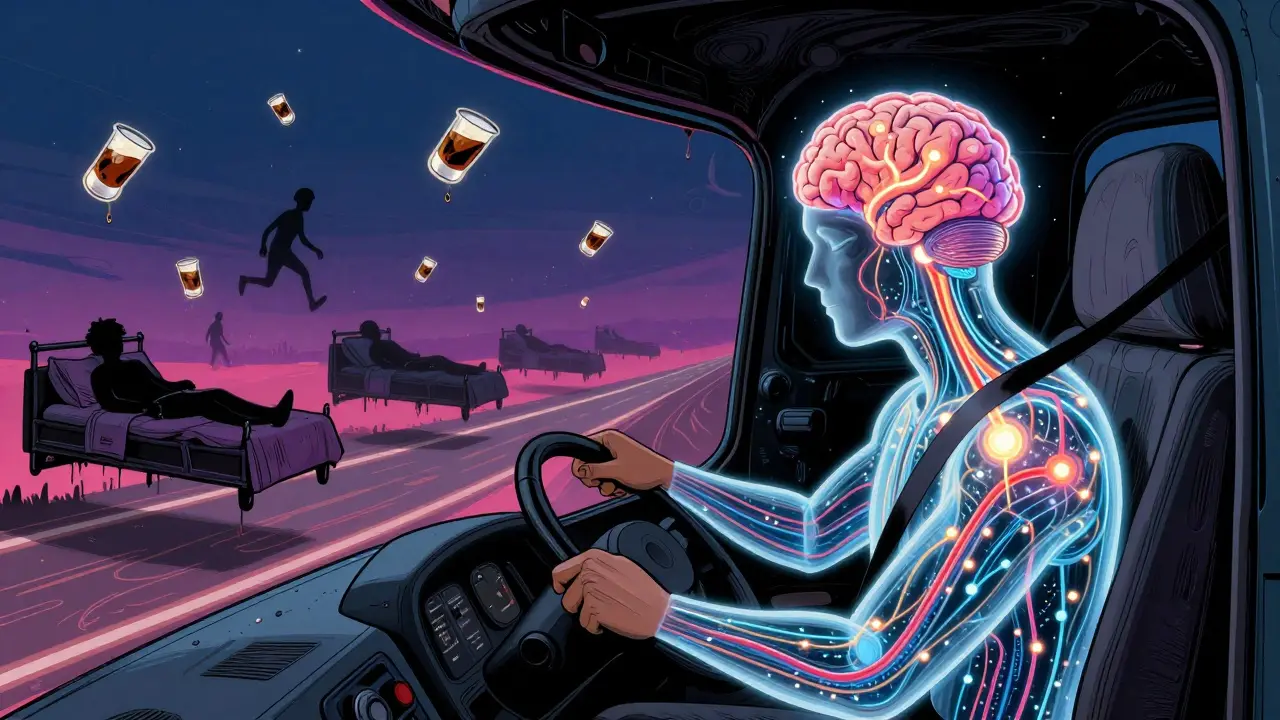
Why Night Shifts Break Your Sleep Clock
Working nights doesn’t just mean sleeping during the day-it means fighting your body’s natural rhythm. Your brain is wired to be awake when it’s light and asleep when it’s dark. When you flip that schedule, your internal clock gets confused. This isn’t just feeling tired-it’s a real medical condition called Shift Work Disorder. The American Academy of Sleep Medicine officially recognized it in 2014, and now we know it affects up to 10 million people in the U.S. alone, especially in healthcare, trucking, and manufacturing.
People on night shifts often report lying awake during the day, then struggling to stay alert at work. That’s not laziness. It’s biology. Studies show night workers are 70% more likely to have accidents on the job. One nurse in Bristol told me she once nodded off while checking a patient’s IV drip. She woke up with the bag nearly empty. That’s the kind of mistake fatigue causes.
What Medications Are Used-and How They Work
There are two main types of medications used by night workers: those that help you sleep during the day, and those that help you stay awake at night.
For sleep, doctors sometimes prescribe eszopiclone (Lunesta), zolpidem (Ambien), or zaleplon (Sonata). These work fast, but they come with serious rules. The FDA says you must be able to sleep for 7 to 8 hours after taking them. If you don’t, you might sleepwalk, drive while asleep, or do other dangerous things without remembering. There were 66 reported cases between 2019 and 2022 of people driving or cooking while asleep after taking these drugs. One nurse in Texas drove 15 miles in her sleep after taking zolpidem. She woke up in her garage, confused and terrified.
For staying awake, modafinil (Provigil) and armodafinil (Nuvigil) are the most common. These aren’t stimulants like caffeine. They work differently-targeting brain chemicals that control alertness. A 2020 study found modafinil improved alertness by 34% in night workers compared to placebo. But here’s the catch: it doesn’t make you as sharp as you’d be during the day. It just helps you avoid the worst of the fog.
Many people also use melatonin, an over-the-counter hormone supplement. It’s not a sleeping pill, but it can help reset your body clock. The best time to take it? Three to four hours before you want to sleep. For a nurse who finishes at 7 a.m. and wants to sleep by 9 a.m., that means taking it at 5 a.m. Too early or too late, and it won’t help.
The Hidden Dangers of Sleeping Pills
Most people think sleeping pills are safe because they’re prescribed. They’re not. The FDA added a Boxed Warning in 2023-its strongest safety alert-for drugs like Lunesta and Ambien. Why? Because they can trigger complex sleep behaviors. People have been known to eat, drive, text, or even have sex while asleep, with no memory of it afterward.
And dependency is real. UCLA Health says doctors rarely prescribe these drugs for more than three to four weeks. After that, they stop working as well, and your body starts to need them just to fall asleep. One Reddit user, a night-shift nurse, wrote: “I’ve been on Ambien for nine months. Now I can’t sleep without it.” That’s not uncommon.
Benzodiazepines like lorazepam or clonazepam are sometimes used off-label, but they’re even riskier. A 2022 study found 25-30% of users become dependent after just a few weeks. And if you mix them with alcohol-even one drink-the risk of overdose or respiratory failure jumps dramatically. The FDA explicitly warns against combining these drugs with alcohol or other sedatives.
Wakefulness Drugs: Helpful, But Not a Cure
Modafinil and armodafinil are the go-to for people who need to stay alert on the job. Truck drivers, ER staff, and air traffic controllers often use them under medical supervision. The National Transportation Safety Board found a 28% drop in fatigue-related crashes among truckers using modafinil.
But here’s what no one tells you: these drugs don’t fix your sleep. They just mask the symptoms. Your body still hasn’t adjusted to the night schedule. You’re still running on borrowed time. A 2022 review in Sleep Medicine Research concluded: “No medication can fully restore circadian function.” That’s the hard truth.
Also, tolerance builds. Some users report diminishing effects after three to four weeks. One long-haul driver on an online forum said, “It worked great at first. After two months, I had to double my dose just to stay awake.” That’s a red flag. Increasing your dose without medical advice is dangerous.
What Really Works: Non-Medication Strategies
If medications are risky and temporary, what’s the alternative? Behavioral changes. The best solution isn’t a pill-it’s a routine.
Light exposure is critical. When you finish your night shift, wear dark sunglasses on your way home. Sunlight tells your brain it’s daytime. That makes it harder to sleep. Blocking it helps. Once home, make your bedroom pitch black. Use blackout curtains. Cover LED lights. Even a small glow can disrupt your sleep.
Stick to a sleep schedule-even on days off. If you sleep from 9 a.m. to 5 p.m. on workdays, try to keep that same window on weekends. Shifting your sleep time by more than an hour or two throws your rhythm off again.
Some companies now give workers light therapy boxes. These mimic sunlight and help reset your internal clock. A 2023 SHRM survey found 73% of large employers now offer them. It’s not magic, but it’s safer than pills.
And don’t underestimate caffeine. A cup of coffee 30 minutes before your shift starts can help. But don’t drink it after 3 a.m.-it can linger in your system for 6-8 hours and ruin your daytime sleep.
How to Talk to Your Doctor
If you’re considering medication, don’t just ask for a script. Bring your schedule. Show your sleep log. Tell your doctor exactly when you work, when you sleep, and what’s going wrong.
Many doctors don’t know how shift work affects sleep. A 2022 study found medical residents received only 4.2 hours of formal training on sleep medication safety during their entire residency. That’s not enough. You have to be your own advocate.
Ask: “What’s the half-life of this drug?” “How long should I wait before driving?” “Is there a risk of sleepwalking?” “Are there non-drug options I should try first?”
Also, tell your doctor if you’re using over-the-counter sleep aids. Many night workers take diphenhydramine (Benadryl) or doxylamine (Unisom) because they’re easy to get. But these cause next-day drowsiness in 18% of users, according to FDA labeling. That’s dangerous if you’re operating machinery or driving.
When Medication Might Be Necessary
There are times when medication makes sense. If you’ve tried everything-light control, sleep hygiene, caffeine-and you’re still exhausted, short-term use under supervision can help you get back on track.
For example, if you’re switching from day shifts to night shifts, a doctor might prescribe melatonin for two weeks to help your body adjust. Or a nurse starting night shifts might use modafinil for the first month while building a new sleep routine.
The key is timing and limits. Take modafinil one hour before your shift. Take melatonin three to four hours before your sleep window. Never take sleep meds without planning for 7-8 hours of uninterrupted sleep. And never use them for more than a few weeks without a plan to taper off.

What to Do If You’re Already Dependent
If you’ve been using sleep aids for months and can’t sleep without them, you’re not alone. But you’re not stuck either.
Start by tracking your sleep and medication use for a week. Write down: what you took, when, how long you slept, how alert you felt the next day. Bring this to your doctor.
Don’t quit cold turkey. That can cause rebound insomnia and anxiety. Work with your doctor on a slow taper. Replace the pill with behavioral tools: dark room, white noise, breathing exercises, or a warm bath before bed.
Support groups like the Circadian Sleep Disorders Network have over 12,500 members who share tips on timing, light exposure, and tapering off meds. You don’t have to do this alone.
Final Safety Checklist
- Never drive or operate machinery within 8 hours of taking a sleep aid.
- Take wake-promoting meds exactly one hour before your shift.
- Take melatonin 3-4 hours before you want to sleep, not right before bed.
- Avoid alcohol with any sleep or wakefulness medication.
- Use blackout curtains and block all light in your bedroom.
- Don’t use OTC sleep aids long-term-they cause drowsiness the next day.
- Track your sleep and alertness daily for at least two weeks.
- See your doctor before starting any new medication, even if it’s over-the-counter.
What’s Coming Next
Researchers are starting to look at genetic testing to predict how individuals respond to sleep meds. Within five years, doctors may be able to say, “Based on your DNA, you metabolize modafinil slowly-so take half the dose.”
The CDC and NIOSH are also developing new guidelines for doctors prescribing to shift workers, expected in mid-2024. These will push for better communication between patients and providers about work schedules.
For now, the best advice is simple: don’t rely on pills to fix your biology. Use them only as a bridge while you build a sustainable sleep routine. Your safety-and the safety of others-depends on it.

lisa Bajram
January 10, 2026 AT 11:57Okay but let’s be real - melatonin at 5 a.m. is a game-changer. I’m a night-shift EMT, and I swear by it. Just don’t take it with a side of pizza and Netflix. 😴✨ My sleep quality went from ‘tossed and turned for 4 hours’ to ‘passed out like a log.’
Paul Bear
January 11, 2026 AT 01:25Modafinil is not a cognitive enhancer - it’s a pharmacological Band-Aid. The 34% improvement cited is statistically significant but clinically negligible. You’re not ‘alert’ - you’re in a chemically induced state of low-grade hyper-vigilance with no REM rebound. The NTSB data is cherry-picked. Fatigue-related crashes dropped because modafinil users were monitored more closely - not because the drug fixed circadian misalignment. This is medicalized denial.
Jaqueline santos bau
January 11, 2026 AT 22:13OMG I just read this and I’m crying 😭 My husband’s a trucker and he’s been on Ambien for 11 months. He drove 20 miles asleep last winter. We almost lost him. I begged him to stop. He said ‘I can’t sleep without it.’ Now I’m scared to let him sleep alone. Who else has been through this??
Kunal Majumder
January 12, 2026 AT 03:24Bro, just start sleeping at the same time every day - even on weekends. I was a nurse for 8 years. Didn’t use a single pill. Sunglasses on the way home, blackout curtains, white noise machine. Done. Your body will adjust. No magic, just consistency. You got this 💪
Aurora Memo
January 12, 2026 AT 10:36This is such an important post. I wish more doctors knew about shift work disorder. I’ve seen patients prescribed benzodiazepines for months without ever being asked about their schedule. We need better education - not just for patients, but for providers too.
chandra tan
January 13, 2026 AT 06:20India has thousands of night shift workers - call center staff, factory workers, security guards. No one talks about this. We don’t have access to modafinil or melatonin. Just chai and willpower. I wish someone would make a simple guide in Hindi or Tamil for people like us.
Dwayne Dickson
January 15, 2026 AT 01:30Let’s be clear: prescribing sleep aids to shift workers is corporate malpractice. Employers don’t want to adjust schedules. They want you to pop a pill and keep working. This isn’t medicine - it’s exploitation dressed in white coats. And yes, I’ve seen the data. The ‘safety’ of modafinil is a marketing myth sold to desperate people.
Ted Conerly
January 15, 2026 AT 21:05If you’re on night shifts, your sleep isn’t broken - your schedule is. Don’t fix your body. Fix your environment. Blackout curtains. No screens after 6 a.m. Cool room. Same bedtime every day. It’s not hard. It’s just hard to start. But once you do? Life changes. I did it. You can too.
Faith Edwards
January 16, 2026 AT 01:08It’s alarming how casually people treat these medications. Melatonin? Over-the-counter. Ambien? Prescribed by a GP who barely knows your name. We’ve normalized chemical dependency in the name of productivity. This isn’t resilience - it’s a slow-motion tragedy. And the FDA’s boxed warning? Too little, too late.
Michael Marchio
January 17, 2026 AT 02:19Let’s not romanticize behavioral strategies. Yes, light exposure helps. Yes, sleep hygiene matters. But for someone working 12-hour night shifts five days a week, with kids, a partner, and a dog, trying to ‘adjust your routine’ is a luxury. You can’t control your environment when your employer controls your schedule. And yes, I’ve tried the blackout curtains. I’ve tried the melatonin. I’ve tried the white noise. I’ve tried everything. And I still wake up at 3 p.m. with my heart racing, my eyes burning, and my brain screaming. Medication isn’t a crutch - it’s a survival tool. And if you’re judging me for using it, you’ve never worked a night shift. You have no idea.
Jake Kelly
January 17, 2026 AT 11:30Thank you for writing this. I’m a new night-shift tech and I was terrified. This gave me hope. I’m starting with the sunglasses and the dark room tonight. No pills yet. Just trying to build a rhythm. Small steps.
Ashlee Montgomery
January 19, 2026 AT 09:02Is it possible that our entire society is built on the illusion of constant availability? We demand 24/7 service - healthcare, delivery, security - but refuse to acknowledge the biological cost. We don’t treat shift workers like humans. We treat them like machines with a reset button. And then we’re shocked when they break.
neeraj maor
January 21, 2026 AT 00:53Modafinil is a CIA drug. They used it in Vietnam. Now it’s in every ER and truck depot. The FDA doesn’t want you to know this, but the real reason they approved it was because the military needed soldiers to stay awake for 72 hours. They didn’t care about circadian rhythms. They cared about mission success. Same thing now. Corporations don’t care if you live - they care if you show up.
Jay Amparo
January 22, 2026 AT 08:09I used to think I was just tired. Then I found out I had Shift Work Disorder. I cried for an hour. Then I started the routine - sunglasses, dark room, same sleep time. Three months later, I haven’t touched a pill. I sleep 6 hours straight. I’m not ‘fixed’ - but I’m alive again. You’re not broken. Your schedule is. Change the schedule, not your brain.
Ritwik Bose
January 22, 2026 AT 14:01Thank you for this. 🙏 I’ve been using melatonin for 2 months. I take it at 4:30 a.m. before my 11 p.m. to 7 a.m. shift. I sleep from 8 a.m. to 4 p.m. I’m not perfect, but I’m sleeping. And I’m alive. 💙