Every year, thousands of people end up in emergency rooms not because of accidents or illness, but because they believed something about their medicine that just wasn’t true. You might think an over-the-counter painkiller is harmless. Or that stopping your antibiotic when you feel better is fine. Maybe you assume natural supplements don’t interact with your prescriptions. These aren’t just harmless myths-they’re dangerous misunderstandings that cost lives.
Myth: Over-the-counter medications are completely safe
It’s easy to think that because you can buy something without a prescription, it’s safe to use however you want. But that’s one of the most deadly misconceptions in medicine. Acetaminophen-the active ingredient in Tylenol and hundreds of other pain relievers and cold medicines-is the leading cause of acute liver failure in the United States. The FDA lowered the recommended daily maximum from 4,000mg to 3,000mg in 2011 after data showed how easily people overdose. Just eight extra-strength tablets (500mg each) hit that limit. Many people don’t realize they’re taking acetaminophen in multiple products at once: a cold medicine, a sleep aid, and a painkiller. That’s how people end up with liver damage without ever meaning to.
Fact: The dose on the label isn’t a suggestion-it’s a limit
Pharmacists don’t pick dosages randomly. Every pill amount, timing, and frequency is based on years of clinical trials, safety studies, and real-world data. Taking more than recommended doesn’t make pain go away faster. It just increases your risk of serious harm. For example, taking more than 1,200mg of ibuprofen in a day raises your chance of stomach bleeding by 4.5 times, according to a 2017 study in JAMA Internal Medicine. The same goes for naproxen, aspirin, and other NSAIDs. Your body doesn’t work better with more of the drug-it just gets overwhelmed. Stick to the label. If it’s not working, talk to your doctor or pharmacist. There’s almost always a safer way.
Myth: You can stop taking your medicine once you feel better
This myth is especially common with antibiotics. You get sick, take your pills, feel better after three days, and decide the rest aren’t necessary. But here’s the problem: the bacteria causing your infection might still be alive. Stopping early doesn’t just mean you could get sick again-it means the toughest bacteria survive, multiply, and become resistant. The CDC estimates that 30% of antibiotic courses are stopped too soon. That’s a big reason why antibiotic-resistant infections now kill 35,000 people in the U.S. every year. The same applies to blood pressure meds, antidepressants, and thyroid pills. Feeling better doesn’t mean the job is done. Finish the full course unless your doctor says otherwise.
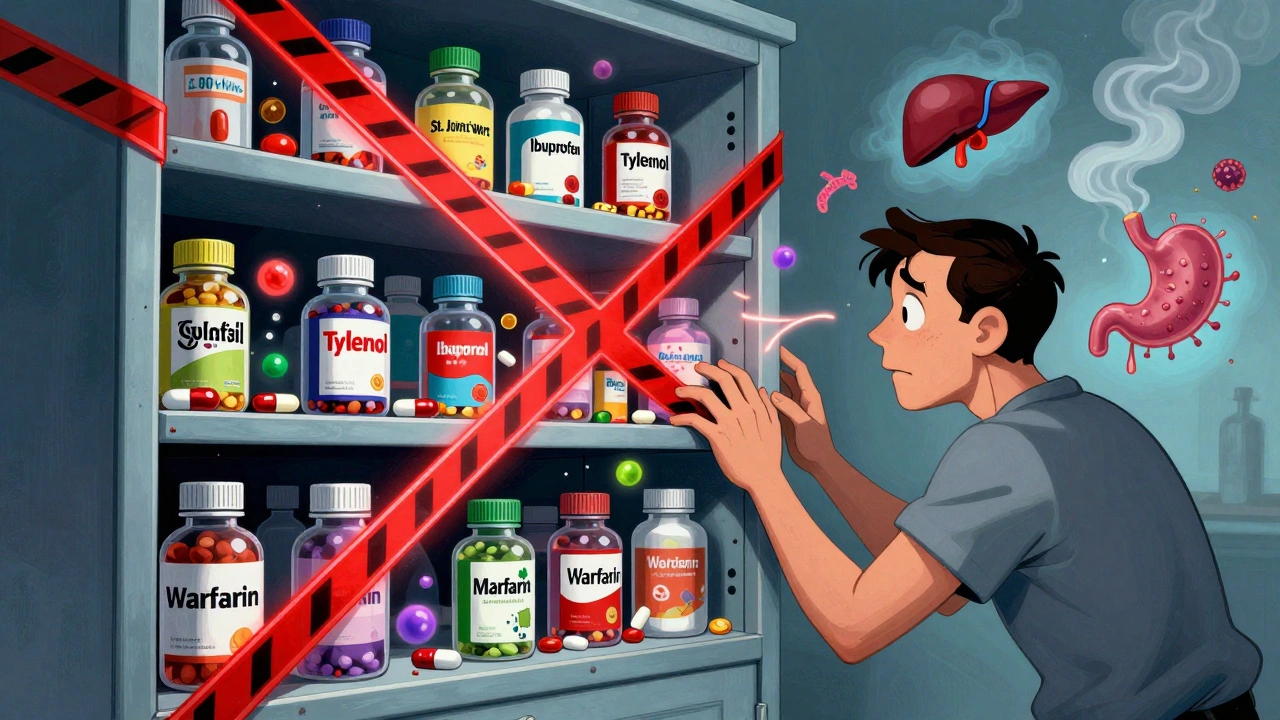
Fact: Herbal and natural supplements can be just as risky as prescription drugs
Many people assume that because something is labeled “natural,” it’s safe. But nature doesn’t care if you’re on other meds. St. John’s Wort, often taken for mild depression, can cut the effectiveness of birth control pills by up to 33%, leading to unintended pregnancies. Ginkgo biloba, popular for memory support, increases bleeding risk by 50% when mixed with warfarin-a blood thinner. Even common supplements like vitamin E and garlic can interfere with clotting. The National Center for Complementary and Integrative Health found that 65% of supplement users believe these products are always safe. That’s not just wrong-it’s dangerous. Always tell your pharmacist about every supplement you take. They can spot interactions you won’t even think to ask about.

Myth: Mixing alcohol with prescription meds is fine if you don’t drink much
“I only have one glass of wine with dinner,” people say. But alcohol doesn’t need to be binge-level to cause harm. When combined with opioids like oxycodone or hydrocodone, even a small amount of alcohol increases the risk of respiratory depression-your breathing slows to a dangerous level-by up to 800%, according to a 2020 study in Addiction Biology. That’s not a slight risk. That’s life-threatening. Alcohol also makes sedatives, sleep aids, and some antidepressants way more powerful than intended. It can spike your blood pressure, crash your blood sugar, or make your liver work overtime. There’s no safe amount for most medications. If your prescription label says “avoid alcohol,” it’s not a suggestion. It’s a warning.
Fact: Generic drugs are just as effective as brand names
Many patients refuse generics because they think they’re “weaker” or “inferior.” That’s not true. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand name. They must also be within 80-125% bioequivalence-meaning your body absorbs them the same way. The American Pharmacists Association confirms that generics work just as well, and they cost up to 80% less. A 2022 study tracking 1.2 million patients found no difference in outcomes between brand-name and generic statins, blood pressure meds, or diabetes drugs. Choosing generics isn’t cutting corners-it’s smart, safe care.
Myth: If your doctor prescribed it, you don’t need to ask questions
Doctors are busy. They might not have time to explain every detail. But that doesn’t mean you shouldn’t ask. Too many patients leave the office with a script and no idea what they’re taking, why, or what to watch for. This silence leads to mistakes. The “Teach-Back Method”-where patients explain their medication plan back in their own words-has been shown to boost understanding from 42% to 89% in clinical studies. If you can’t explain your meds clearly, you’re at risk. Ask: “What’s this for?” “What happens if I miss a dose?” “What side effects should I watch for?” “Can this interact with anything else I take?” These aren’t annoying questions. They’re essential.
Fact: A simple “brown bag review” can prevent 63% of medication errors
Most people have at least five medications-some prescription, some OTC, some supplements. No one remembers them all. That’s why pharmacists recommend bringing everything you take to your doctor or pharmacist once a year. Put it all in a brown bag-pills, liquids, patches, vitamins-and walk in. This “brown bag review” helps uncover duplicates, interactions, expired meds, or doses that are too high. A 2021 study in the Journal of the American Pharmacists Association found this simple step reduced medication discrepancies by 63%. It’s not glamorous. But it’s one of the most effective safety tools you have.
Fact: Synchronizing your refills cuts missed doses by nearly 30%
Managing multiple prescriptions with different refill dates is a nightmare. One runs out on Monday, another on Wednesday, another on Friday. People skip doses because they’re out of pills. ExactCare Pharmacy tracked 5,000 Medicare patients and found that when all prescriptions were aligned to one weekly refill day, adherence jumped from 52% to 81%. That’s a massive improvement. Most pharmacies offer this service for free. Ask for it. It’s not about convenience-it’s about staying healthy.
Fact: Technology is helping patients avoid dangerous mistakes
Apps like Medisafe send reminders, track interactions, and flag potential overdoses. Amazon Pharmacy’s “Ask a Pharmacist” feature has answered over 1.2 million questions about medication safety in 2023 alone-with 94% user satisfaction. The FDA is also updating OTC labels to make overdose warnings clearer, especially for acetaminophen. These tools aren’t magic, but they help. If you’re forgetful or on multiple meds, consider using one. It’s like having a pharmacist in your pocket.
What you can do today
- Check your medicine cabinet. Are there expired pills? Duplicate meds? Unlabeled bottles?
- Bring all your medications (including supplements) to your next appointment.
- Ask your pharmacist: “Is there anything here I shouldn’t mix?”
- Set phone reminders for your meds-don’t rely on memory.
- Don’t stop or change a dose without talking to your doctor or pharmacist first.
Medication safety isn’t about being perfect. It’s about being aware. A few simple steps can keep you out of the hospital and alive longer. The truth is, most medication errors aren’t caused by bad doctors or bad pharmacies. They’re caused by misinformation. You don’t need to be a medical expert. You just need to ask questions, listen, and take the facts seriously.
Can I take more than the recommended dose of ibuprofen if my pain is bad?
No. Taking more than 1,200mg of ibuprofen in 24 hours increases your risk of stomach bleeding by 4.5 times, according to a 2017 JAMA Internal Medicine study. It won’t help more-it just makes you sicker. Talk to your doctor instead. They may recommend a different treatment or adjust your dose safely.
Are herbal supplements always safe because they’re natural?
No. Many herbal products interact dangerously with prescription medications. St. John’s Wort can make birth control fail. Ginkgo biloba increases bleeding risk with blood thinners like warfarin. The National Center for Complementary and Integrative Health found 65% of supplement users believe these are always safe-but that’s a myth. Always tell your pharmacist what you’re taking, even if it’s “just a supplement.”
Why does my doctor say I need to finish my antibiotics even if I feel better?
Stopping antibiotics early leaves behind the strongest bacteria, which then multiply and become resistant to treatment. The CDC says 30% of antibiotic courses are stopped too soon, contributing to 35,000 U.S. deaths each year from drug-resistant infections. Finishing the full course kills all the bacteria, not just the ones making you feel bad.
Is it safe to drink alcohol with my pain medication?
It depends on the medication, but with opioids like oxycodone or hydrocodone, even one drink can increase the risk of dangerous breathing problems by 800%. Alcohol also makes sedatives, sleep aids, and some antidepressants stronger than intended. The safest answer is no-avoid alcohol entirely unless your doctor says otherwise.
Are generic drugs less effective than brand names?
No. The FDA requires generics to have the same active ingredient, strength, and absorption rate as brand-name drugs. Studies tracking millions of patients show no difference in outcomes for blood pressure, cholesterol, or diabetes meds. Generics are cheaper, not weaker. Choosing them saves money without sacrificing safety or effectiveness.
What should I do if I think I’ve taken too much of a medicine?
Call Poison Control immediately at 1-800-222-1222 (U.S.) or your local emergency number. Don’t wait for symptoms. With acetaminophen, liver damage can start without noticeable signs for hours. If you’re unsure what you took or how much, bring the bottle with you to the ER. Time matters.
If you’re on multiple medications, take one small step today: gather all your pills into a bag and bring them to your next appointment. That one action could prevent a hospital visit. Medication safety isn’t complicated-it’s about paying attention, asking questions, and trusting the facts over the myths.
Taya Rtichsheva
December 8, 2025 AT 21:09so i took 3 tylenol with my wine last night and nothing happened lol guess im just immune to liver failure
Evelyn Pastrana
December 10, 2025 AT 01:04my grandma took 12 ibuprofen because her knee hurt and now she's fine. she also eats raw garlic for flu and never gets sick. maybe the science is just for people who don't believe in grandma medicine 🤷♀️
Nikhil Pattni
December 10, 2025 AT 16:58you guys are missing the real issue. in india we have this thing called "chai therapy" where you drink hot tea with turmeric and black pepper and then your body just resets. no meds needed. also i take ashwagandha with my blood pressure pills and my doc says it's fine. why? because my ayurvedic uncle said so. science is just western propaganda anyway. also i once took 1000mg of vitamin c with my antidepressants and felt like a superhero. the FDA doesn't know what they're talking about. you need to think outside the pill bottle. also, i have a PhD in biochemistry so i know better.
Elliot Barrett
December 11, 2025 AT 20:12this article is just fearmongering. if you're dumb enough to mix alcohol with opioids, you deserve to die. stop babying people.
Andrea Beilstein
December 12, 2025 AT 06:59we treat medicine like it's magic when really it's just chemistry and biology. we're scared of our own bodies. we want to believe there's a pill for everything and that we can outsmart nature. but nature doesn't care about our convenience. it just responds. if you take too much, you break. if you stop too soon, the bacteria win. it's not complicated. we just don't want to accept that we're not in control.
Sabrina Thurn
December 12, 2025 AT 16:33the brown bag review is the single most underutilized tool in healthcare. i work as a clinical pharmacist and i've seen people bring in 17 different bottles - some expired, some duplicates, some with no labels. one guy had four different acetaminophen products and didn't realize they all contained the same ingredient. after we did the review, we cut his meds by 40%. he hasn't been to the ER in two years. if you're on more than three meds, do this. it's free. it's simple. it saves lives.
Richard Eite
December 13, 2025 AT 06:54generic drugs are just as good. period. america wastes billions on brand names because we're lazy and gullible. if you're still paying extra, you're being scammed. #americanhealthcare #buygeneric
Tim Tinh
December 13, 2025 AT 14:16just wanted to say i started using medisafe after my aunt had a bad reaction to mixing her supplements with her heart meds. best decision ever. i get texts reminding me to take my blood pressure pill and it tells me if something might clash. i used to forget half the time. now i'm on track. also, i asked my pharmacist about my fish oil and she said it's fine with my blood thinner - but only if i take it with food. small stuff like that matters. thanks for the article, it made me check my cabinet. i found three expired pills i'd forgotten about 🙃
Stacy Tolbert
December 14, 2025 AT 12:57i took my antidepressants for 3 weeks and felt worse so i stopped. now i'm in therapy and i feel like a broken person. why didn't anyone tell me it takes 6 weeks to work? i feel so alone in this.
Ryan Brady
December 15, 2025 AT 23:06st john's wort messes with birth control? lol no wonder so many girls are pregnant. they think herbal = safe. dumbass culture.
Raja Herbal
December 16, 2025 AT 01:09in india we say "dawa ka dose, doctor ka hukum" - medicine dose is the doctor's command. you don't stop antibiotics just because you feel better. we learn this in school. why is america so confused?
Iris Carmen
December 16, 2025 AT 04:41i just checked my cabinet and found a bottle of codeine from 2018. i forgot i even had it. i threw it out. small win.
Delaine Kiara
December 17, 2025 AT 18:31my doctor gave me a script for a generic and i refused because i thought it was "cheap medicine." i didn't know it was the same thing. now i feel like an idiot. also my mom cried when she found out i was taking ginkgo with warfarin. i didn't even know it was a thing. this article made me want to cry and hug my pharmacist.