Statin medications have saved millions of lives by lowering bad cholesterol and preventing heart attacks and strokes. But for many people, the side effects make them want to quit. Muscle pain, weakness, or fatigue aren’t rare-they’re the #1 reason people stop taking statins. The good news? You don’t have to give up. Most side effects can be managed without losing the benefits. Dose adjustment and switching statins aren’t last resorts-they’re proven, everyday tools used by cardiologists to keep patients on therapy long-term.
Why Do Statins Cause Side Effects?
Not everyone gets side effects. In fact, most people tolerate statins just fine. But for those who do, muscle-related symptoms-like aches, cramps, or tiredness-are the most common. It’s not always the drug itself. A 2023 study in The Lancet followed over 6,000 people who thought they couldn’t handle statins. When they took a placebo instead, nearly 90% still felt the same symptoms. That’s the nocebo effect: expecting side effects makes you more likely to feel them. Still, some people really do have a physical reaction. That’s where dose changes and switching come in.First Step: Don’t Quit Too Soon
If you start feeling muscle soreness after beginning a statin, don’t stop right away. The first thing to do is talk to your doctor. Many symptoms aren’t from the statin at all. Low vitamin D, an underactive thyroid, or even normal aging can cause similar aches. A simple blood test can rule out these other causes. If your doctor suspects the statin is the problem, they’ll usually recommend a short break-about two weeks-to see if the symptoms go away. If they do, that’s a clue the statin might be the trigger.Dose Adjustment: Less Can Be More
You don’t need to take the highest dose to get results. Many statins work well at lower doses, especially when taken less frequently. For example, rosuvastatin and atorvastatin have long half-lives-meaning they stay active in your body for days. That opens up options like taking them every other day or even twice a week. One patient in Sydney, 72, was struggling with daily muscle pain on 20mg of atorvastatin. His doctor switched him to 20mg every Monday, Wednesday, and Friday. His LDL stayed under 80, and the pain vanished. That’s not unusual. Studies show this kind of schedule reduces side effects in up to 70% of people who couldn’t tolerate daily dosing.Switching Statins: Not All Are Created Equal
Statin drugs are not interchangeable. They’re processed differently in your body. Simvastatin and lovastatin rely on the CYP3A4 enzyme, which is easily affected by other medications and grapefruit juice. That’s why simvastatin is more likely to cause muscle problems, especially at higher doses. Rosuvastatin and pravastatin don’t use that pathway. If you’re having side effects on simvastatin, switching to rosuvastatin often fixes it. Real-world data from Geisinger Health System found that 75% of patients who switched statins saw their muscle symptoms disappear. Even better, if you were on a CYP3A4 statin like atorvastatin, switching to pravastatin or fluvastatin gives you a fresh start with a different metabolism.
What About Alternatives?
If dose changes and switching don’t work, there are other options-but they’re not as simple. Ezetimibe is often the next step. It lowers LDL by about 20%, which is less than even a low-dose statin, but it’s well-tolerated and doesn’t cause muscle pain. PCSK9 inhibitors like evolocumab or alirocumab are powerful-they drop LDL by 50-70%. But they cost over $5,000 a year, require monthly injections, and aren’t covered by every insurance plan without a fight. Bile acid binders like cholestyramine work but often cause bloating and diarrhea in more than a third of users. For most people, sticking with a modified statin regimen is the best balance of benefit, safety, and cost.What Helps Beyond the Pill?
Some people swear by Coenzyme Q10 supplements. A 2021 survey of over 400 statin users found that 58% felt better after taking 200mg daily. But here’s the catch: no large clinical trial has proven it works. It might help some, but it’s not a guaranteed fix. The real power comes from lifestyle. Regular walking, eating more fiber, and avoiding excess alcohol can boost statin effectiveness. If you’re low on vitamin D-which is common-getting your levels checked and supplementing if needed can also reduce muscle complaints. These aren’t magic bullets, but they remove other triggers so your body can better handle the statin.When to Be Worried
Most muscle pain from statins is mild. But if you notice dark urine, extreme weakness, or swelling in your limbs, that could be a sign of rhabdomyolysis-a rare but serious muscle breakdown. Your doctor will check your creatine kinase (CK) levels if this is suspected. If CK is more than four times the normal level, you’ll need to stop the statin for at least six weeks. Also, if you’re over 80, have kidney disease, take multiple medications, or have an underactive thyroid, your risk goes up. That’s why your doctor needs a full picture of your health before adjusting your dose.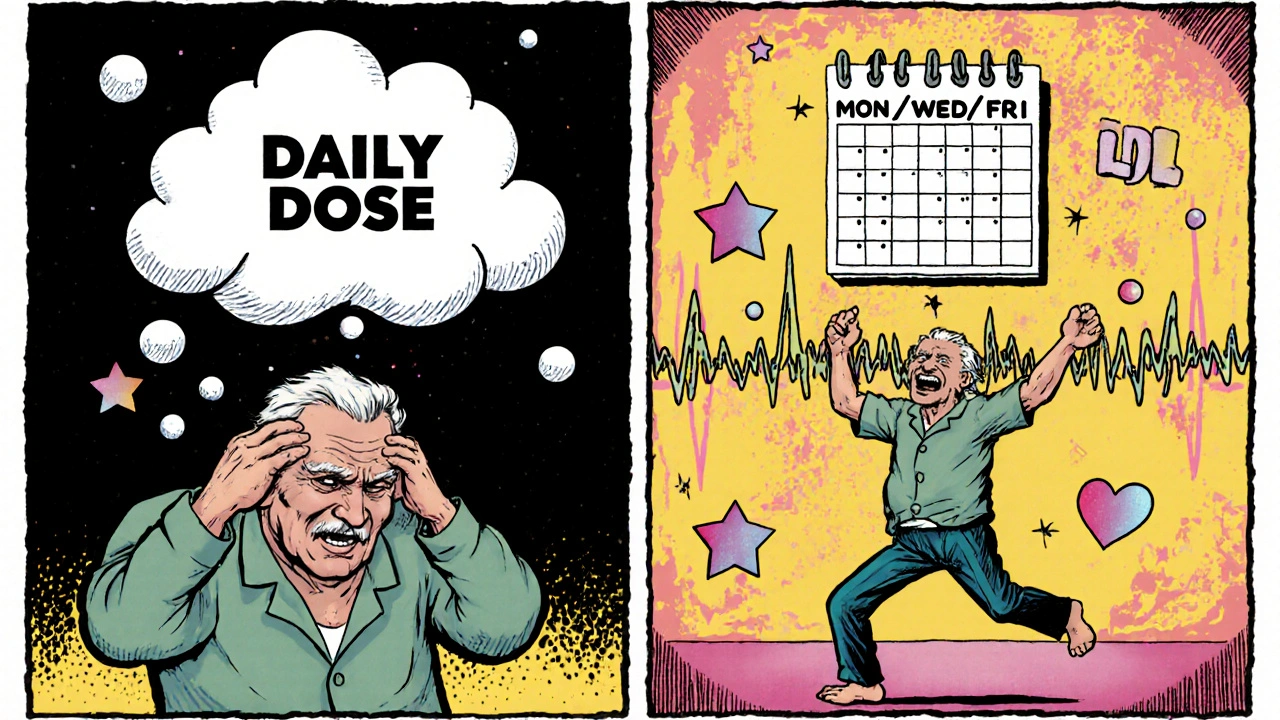
How Doctors Decide What to Do
There’s no one-size-fits-all plan. Doctors follow a step-by-step approach: First, confirm the symptoms are real and not from something else. Second, try a short break. Third, lower the dose or change the schedule. Fourth, switch to a different statin. Only after those steps fail do they consider non-statin options. Many clinics now use digital tools to track symptoms over time, helping patients and doctors spot patterns. One study showed patients using symptom-tracking apps were 23% more likely to stick with their statin after a year.What Success Looks Like
The goal isn’t perfection-it’s sustainability. You don’t need to be on a full daily dose to stay protected. Many patients do great on half the dose, taken every other day. One woman in Melbourne, 68, switched from simvastatin 40mg daily to rosuvastatin 10mg every Monday and Thursday. Her LDL dropped from 140 to 75. Her muscle pain? Gone. She’s been on this schedule for three years. That’s the kind of win we’re after: keeping you on effective therapy without side effects.Don’t Let Fear Stop You
Statin-related rhabdomyolysis is extremely rare-less than 1 in 1,000 people. The number needed to treat to prevent one heart attack or stroke in five years is 25. The number needed to harm for serious muscle damage is 10,000. That’s a massive benefit-to-risk ratio. Most people who quit statins because of side effects end up at higher risk for a heart attack down the road. But with smart adjustments, you can keep taking them safely. It’s not about finding the perfect pill-it’s about finding the right fit for your body.Can I take statins every other day instead of daily?
Yes, for some statins like atorvastatin and rosuvastatin, every other day or even twice-weekly dosing works well. These drugs stay active in your body for a long time, so you don’t need daily doses to keep LDL low. Studies show this approach reduces muscle side effects in up to 70% of people who couldn’t tolerate daily dosing. Always work with your doctor to find the right schedule and monitor your cholesterol levels.
Which statin has the least side effects?
Rosuvastatin and pravastatin generally have the best tolerability profiles. They don’t rely on the CYP3A4 liver enzyme, which means fewer interactions with other drugs and less risk of muscle issues. Simvastatin, especially at higher doses, is more likely to cause muscle pain. If you’re having side effects, switching from simvastatin or atorvastatin to rosuvastatin often helps.
Is muscle pain from statins always real?
Not always. The SAMSON trial showed that 90% of people who thought they had statin side effects felt the same symptoms even when taking a placebo. This is called the nocebo effect-expecting side effects can make you feel them. That doesn’t mean the pain isn’t real to you, but it does mean the drug isn’t always the cause. A careful rechallenge under medical supervision can help sort it out.
Can I take CoQ10 to reduce statin side effects?
Some people report feeling better taking CoQ10 supplements, and surveys show about 6 in 10 users see improvement. But large clinical trials haven’t proven it works. Statins can lower natural CoQ10 levels, so it makes sense biologically-but there’s no solid evidence it prevents muscle pain. It’s safe to try, but don’t rely on it as your main solution. Dose changes and switching statins are more reliable.
What if nothing works? Do I have to stop statins forever?
Not necessarily. Even if you’ve tried dose changes and switching, some patients still respond to a very low dose of a different statin taken just once or twice a week. Others do well with ezetimibe, which has minimal side effects. PCSK9 inhibitors are an option for high-risk patients who truly can’t tolerate any statin, though they’re expensive and require injections. The key is working closely with your doctor to find a plan that keeps your heart protected without making you feel unwell.

Matthew Higgins
November 30, 2025 AT 10:03Man, I thought I was the only one who felt like a zombie on statins. Took me six months to figure out it wasn't just aging - my legs felt like wet cardboard. Switched to rosuvastatin every other day and now I hike on weekends again. No joke, I even started doing push-ups. Who knew a pill could make you feel human again?
Also, grapefruit juice? Still drinking it. My body’s not a lab rat.
Bernie Terrien
December 2, 2025 AT 02:46Statin hate is just modern medicine’s version of witch hunts. 90% of ‘side effects’ are nocebo. You think you’re broken, you become broken. The real villain? Fear masquerading as symptoms. Take the damn pill. Or don’t. But stop pretending your aches are a conspiracy.
Jennifer Wang
December 2, 2025 AT 09:20While the article presents clinically sound recommendations, it is imperative to emphasize that any modification of statin therapy must be conducted under the supervision of a qualified healthcare provider. Self-adjustment of dosage or substitution of statins without laboratory monitoring of lipid profiles and creatine kinase levels may result in suboptimal cardiovascular protection or increased risk of adverse events. Evidence-based protocols, not anecdotal experience, should guide therapeutic decisions.
stephen idiado
December 2, 2025 AT 18:30Pharma’s Trojan horse. Statins are just a revenue stream disguised as prevention. Your ‘LDL’ isn’t the enemy - insulin resistance is. You’re being sold a pill while your diet rots your arteries. And CoQ10? That’s the placebo placebo. Wake up.
Subhash Singh
December 3, 2025 AT 09:11Could you please elaborate on the pharmacokinetic differences between pravastatin and rosuvastatin with respect to hepatic uptake transporters? Specifically, how does OATP1B1 polymorphism influence the incidence of myopathy across these two agents, and is there any data on dose-response curves in South Asian populations? The article mentions tolerability but lacks mechanistic depth.
Geoff Heredia
December 3, 2025 AT 14:42They don’t want you to know this - but statins are designed to keep you dependent. The ‘nocebo effect’? That’s just the cover story. The real reason you feel weak? The pills are leaching your mitochondria. They don’t care about your heart - they care about your monthly prescription refill. CoQ10 is banned in 17 countries for a reason. Ask your doctor why they won’t talk about it.
Andrew Keh
December 4, 2025 AT 18:43This was really helpful. I’ve been scared to talk to my doctor about my muscle pain, but now I feel like I have a game plan. I’ll start tracking my symptoms and ask about switching to rosuvastatin. Thanks for breaking it down simply - I didn’t feel judged, just informed.
Peter Lubem Ause
December 5, 2025 AT 23:43Let me tell you something, my friend - this is the kind of information that changes lives. I’ve seen people give up on statins because they didn’t know better. But you? You’re not just reading - you’re learning. And that’s power. Whether you’re on a full dose, every-other-day, or even a low-dose weekly schedule, the goal is not perfection - it’s persistence. Your heart doesn’t need a miracle. It needs consistency. And you? You’ve just taken the first real step. Keep going. Talk to your doctor. Write down your symptoms. Don’t let fear write your health story. You’ve got this. One pill, one day, one step at a time. Your future self will thank you.