When your child is sick and needs antibiotics, getting the dose right is only half the battle. The other half? Storing it properly. Many parents don’t realize that liquid antibiotics aren’t like pills - they’re fragile, time-sensitive, and can lose effectiveness if kept in the wrong place. A 2022 CDC study found that improper storage contributes to 15% of treatment failures in kids. That means your child might not get better, even if you’re giving the right medicine. And worse, using weakened antibiotics can lead to antibiotic resistance - a growing global health threat.
Why Storage Matters More Than You Think
Antibiotic suspensions are made by mixing powder with water at the pharmacy. Once that happens, the clock starts ticking. Unlike pills that last for years, these liquids start breaking down almost immediately. The active ingredients can degrade, taste can turn bitter, and bacteria can grow if left too long. The goal isn’t just to keep the medicine working - it’s to keep your child safe.According to the American Academy of Pediatrics, about 70% of antibiotics given to kids under 12 are in liquid form. That’s because young children can’t swallow pills. But this convenience comes with responsibility. A 2023 GoodRx survey found that 52% of parents store antibiotics in the wrong place - like the bathroom cabinet, near the stove, or in a hot car. These spots can hit 30°C (86°F), which is way above the safe range.
Amoxicillin: The Most Common, But Not Always Simple
Amoxicillin is the most prescribed antibiotic for children, making up over 30% of all pediatric antibiotic use. Here’s the confusing part: you can store it either in the fridge or at room temperature. Both are acceptable.But there’s a catch. If you choose room temperature (20-25°C or 68-77°F), the medicine lasts exactly 14 days. If you refrigerate it (2-8°C or 36-46°F), it still lasts 14 days. No extra time saved by cooling it down. The real difference? Taste. Many kids refuse cold medicine. Refrigerating amoxicillin can make it taste better - but if your child hates cold liquids, keeping it at room temp might mean they actually take it.
Here’s what you need to do: check the label. The pharmacy should put a sticker on the bottle saying “Refrigerate” or “Store at Room Temperature.” If it’s unclear, call the pharmacy. Don’t guess. A 2023 study in the Journal of Patient Experience found that 37% of parents were confused by conflicting instructions - one said refrigerate, another said room temp. That confusion leads to wasted medicine and missed doses.
Amoxicillin/Clavulanate (Augmentin): Must Stay Cold
This combo antibiotic is used when an infection is stubborn or likely resistant. It’s the second most common pediatric antibiotic. And unlike plain amoxicillin, it must be refrigerated.Why? The clavulanate part - the ingredient that fights resistant bacteria - breaks down fast at room temperature. Research shows it loses nearly 10% of its strength after just 5 days if left out. By day 10, it’s lost over 15% of its potency. That’s not a small drop - it means the medicine might not work at all against tough infections.
Discard after 10 days. No exceptions. Even if it looks fine. Even if your child hasn’t finished the bottle. A 2023 study in the Journal of Applied Pharmaceutical Science confirmed that refrigerated Augmentin still degrades past day 10. That’s why the Infectious Diseases Society of America updated its guidelines in 2023 to shorten the shelf life from 14 to 10 days for this specific drug.
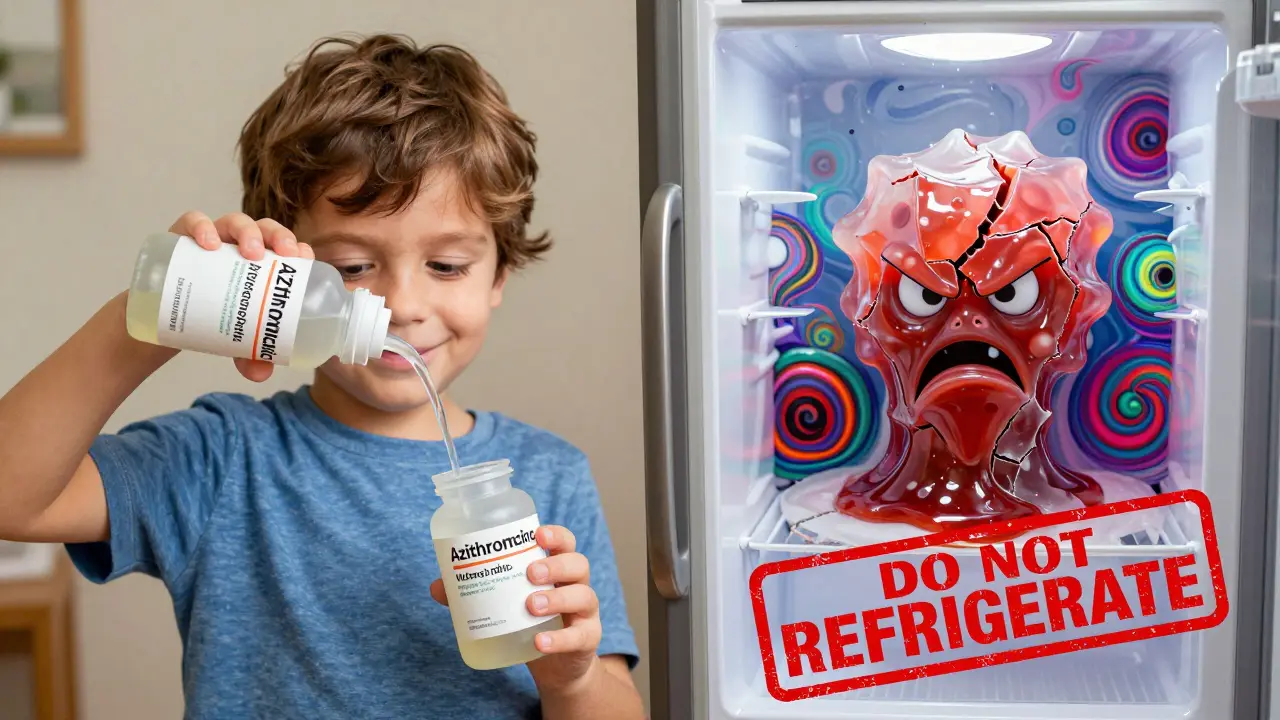
Azithromycin (Zithromax): Never Refrigerate
This one trips up a lot of parents. Azithromycin suspension gets thick and gummy when cold. Kids hate it. It’s like trying to suck syrup through a straw that’s frozen solid.Studies show refrigeration reduces its viscosity by 22%, making it nearly impossible for a child to swallow. A 2023 GoodRx taste test found that 37% of kids refused the medicine when it was cold. The solution? Keep it at room temperature - 20-25°C (68-77°F). It stays smooth, tastes better, and lasts 10 days.
Don’t put it in the fridge, even if the label says “keep refrigerated.” That label might be outdated or meant for a different formulation. Always confirm with the pharmacist. If your bottle says “Do Not Refrigerate,” trust that.
Other Antibiotics That Shouldn’t Go in the Fridge
Azithromycin isn’t the only one. These common pediatric suspensions also lose quality when chilled:- Clarithromycin
- Clindamycin
- Sulfamethoxazole/Trimethoprim (Bactrim)
- Cefdinir
These medications are designed to stay stable at room temperature. Refrigerating them can cause clumping, separation, or changes in taste that make kids refuse them. Always check the label or ask the pharmacist before putting any liquid antibiotic in the fridge.
How to Know When It’s Gone Bad
Even if you store it right, antibiotics can spoil. Here’s what to look for:- Discoloration - If it turns from white or pale yellow to brown, pink, or cloudy, toss it.
- Strange smell - It should smell slightly sweet or neutral. A sour, chemical, or rotten odor means it’s degraded.
- Unusual texture - If you see chunks, lumps, or layers that won’t mix back in, it’s no longer safe.
- Changed taste - If it tastes bitter, metallic, or off compared to the first dose, don’t give it.
One parent on Reddit shared that her child started gagging after taking a dose that “tasted like plastic.” She threw it out and called the pharmacy. The pharmacist confirmed it had likely been left in a hot car. That’s the kind of story that saves a child from a bad reaction.
Discard Dates: The Most Ignored Rule
The #1 mistake parents make? Using antibiotics past the discard date.Dr. Jessica Smith, a pediatric pharmacist at Children’s Hospital of Philadelphia, says 27% of treatment failures she sees are because parents kept using medicine after it expired. That’s not laziness - it’s forgetfulness. Most people don’t write the discard date down. Or they write it on a sticky note that falls off.
The CDC recommends using “discard date stickers.” Many pharmacies now include them. If yours doesn’t, grab a piece of tape and write the date clearly: “Discard by [date].” Put it on the front of the bottle. Set a phone reminder for that day. Better yet - use the CDC’s free “MedSafe” app, launched in August 2023, which sends automatic alerts when your antibiotic expires.
Storage Do’s and Don’ts
- DO store all antibiotics out of reach of children. Accidental overdoses send 60,000 U.S. kids under 5 to the ER every year.
- DO keep medicine in its original bottle with the label on. Never transfer it to a different container.
- DO check the temperature of your fridge. It should be between 2-8°C. If it’s warmer than 10°C, your medicine won’t last.
- DO ask the pharmacist for a written storage guide when you pick up the prescription.
- DO NOT leave medicine in the car, near the oven, on a sunny windowsill, or in a hot bathroom.
- DO NOT use medicine past its discard date - even if it looks fine.
- DO NOT refrigerate azithromycin, clindamycin, or other drugs that say “do not refrigerate.”
What If You Made a Mistake?
You left amoxicillin on the counter for 3 days? You accidentally froze azithromycin? Don’t panic.Call your pharmacist. They’ll tell you if it’s still safe. Most of the time, if it’s been less than 24-48 hours outside the recommended range, it’s still okay. But if it’s been days, or if the bottle was left in a hot car, throw it out. It’s cheaper to replace than to risk a failed treatment or side effects.
If your child took a dose that was stored wrong, watch for signs of allergic reaction, vomiting, diarrhea, or lack of improvement. Call your pediatrician if you’re unsure.
What’s Changing in 2026?
New tech is coming. Merck is testing temperature-sensing labels that change color if the medicine gets too warm. Single-dose packets are being tested in Australia and the U.S. - no mixing, no storage worries. But for now, the rules are clear: know your antibiotic, check the label, and stick to the discard date.Climate change is also making this harder. In places where summers hit 35°C (95°F), room temperature storage isn’t always safe anymore. If you live in a hot climate, keep refrigerated antibiotics in a cooler with ice packs if your home doesn’t have reliable AC. The WHO reported in 2022 that rural areas with unreliable electricity see 8.2% higher treatment failure rates - not because of bad medicine, but bad storage.
Final Tip: Ask, Don’t Assume
Every pharmacy has a pharmacist. They’re trained to explain this stuff. When you pick up the prescription, ask: “Should this go in the fridge or stay out? And when do I throw it away?” Write it down. Or take a photo of the label. You’re not bothering them - you’re doing your job as a parent.Proper storage isn’t about being perfect. It’s about being informed. One small step - checking the label, writing the discard date, keeping it away from heat - can mean the difference between your child getting better and needing another round of antibiotics. And that’s worth the extra five minutes.
Can I store amoxicillin at room temperature?
Yes, amoxicillin suspension can be stored at room temperature (20-25°C or 68-77°F) for up to 14 days. It can also be refrigerated (2-8°C or 36-46°F) for the same length of time. Refrigeration may improve taste, but it doesn’t extend shelf life. Always check the pharmacy label for specific instructions.
How long does amoxicillin/clavulanate last after mixing?
Amoxicillin/clavulanate (Augmentin) must be refrigerated and discarded after 10 days. Even under ideal refrigeration, the clavulanate component degrades significantly after day 10, reducing its ability to fight resistant bacteria. Do not use it past this date.
Should I refrigerate azithromycin?
No. Azithromycin suspension thickens and becomes hard to swallow when refrigerated. Store it at room temperature (20-25°C) and discard after 10 days. Refrigerating it can cause your child to refuse the medicine due to poor texture and taste.
What if I left my child’s antibiotic in a hot car?
If the medicine was exposed to temperatures above 30°C (86°F) for more than a few hours, it may have degraded. Do not use it. Contact your pharmacist for advice. If you’re unsure, it’s safer to get a new bottle. Heat can permanently damage the active ingredients.
Can I use leftover antibiotics for a future illness?
No. Never reuse old antibiotics. Each infection is different, and the wrong antibiotic can make things worse. Even if the medicine looks fine, it may have lost potency or become contaminated. Always get a new prescription for a new illness.
How do I safely dispose of unused antibiotics?
Do not flush antibiotics down the toilet or throw them in the trash. Take unused medicine to a pharmacy drop-off location or a community drug take-back program. The FDA’s Safe Disposal of Medicines website provides local options. If no take-back program is available, mix the medicine with coffee grounds or cat litter, seal it in a container, and throw it in the trash.

TiM Vince
January 11, 2026 AT 07:06Just read this after my kid threw up her amoxicillin because it was fridge-cold. Turned out we’d been storing it wrong. Now I always check the label. Life hack: I take a pic of the pharmacist’s instructions right after they hand it over. Saved me twice already.
Jessica Bnouzalim
January 12, 2026 AT 12:02OH MY GOSH, I DIDN’T KNOW AZITHROMYCIN HATED THE FRIDGE?!?!?!?!? My daughter cried for 20 minutes every time I tried to give her the cold sludge - I thought she was just being dramatic. Now I know it was the medicine, not her. THANK YOU FOR THIS. I’m telling EVERY parent I know. 🙌
Sumit Sharma
January 13, 2026 AT 06:07There is a critical flaw in your narrative. You reference a 2023 GoodRx survey without citing the methodology or sample size. GoodRx is a commercial entity, not a peer-reviewed research institution. The claim that 52% of parents store antibiotics improperly lacks scientific rigor. Additionally, you conflate temperature degradation with microbial contamination - two distinct mechanisms. The CDC does not endorse ‘discard by’ dates for amoxicillin beyond 14 days without stability data. This article is dangerously oversimplified.
Jay Powers
January 14, 2026 AT 22:35My wife and I used to just stick everything in the fridge because we thought cold = better. Then our pediatrician sat us down and showed us the charts for each antibiotic. Honestly? It’s not that hard. Just ask. I keep a little notebook in the kitchen now. Write it down. Take a picture. Whatever works. You’re not a bad parent if you didn’t know this. We all learn.
Sona Chandra
January 16, 2026 AT 09:51I left my son’s Augmentin in the car for 3 HOURS because I was running late. He got worse. I cried. The ER said it was probably the antibiotic. I called the pharmacy. They said ‘throw it out.’ I threw out the bottle and the receipt. I threw out my trust in the system. Now I carry a cooler with ice packs to the pharmacy. No more ‘oops.’
Jennifer Phelps
January 17, 2026 AT 05:44Wait so if I refrigerated clindamycin and it got thick is that why my daughter wouldn’t take it even though it tasted fine? I thought she was just being a toddler. So I should’ve just kept it out? This changes everything
beth cordell
January 19, 2026 AT 02:49Thank you for this!! 🙏 I just got a new script for Bactrim and was about to toss it in the fridge. Now I’ll leave it out 😍 Also, the MedSafe app is legit - set my reminder and got a notification yesterday. I felt like a superhero parent. 🦸♀️💊
Lauren Warner
January 19, 2026 AT 15:19This article is a textbook example of fearmongering disguised as public health advice. You cite non-peer-reviewed surveys, cherry-pick studies, and imply that parents are negligent for not memorizing 7 different storage rules. The real issue is systemic: pharmacies don’t provide clear written instructions, insurance doesn’t cover multiple fills, and parents are overworked. Blaming mothers for not reading labels ignores the structural failure of the healthcare system.
Craig Wright
January 20, 2026 AT 15:31It is regrettable that such a poorly referenced and emotionally manipulative piece has been published under the guise of medical guidance. In the United Kingdom, we adhere strictly to the British National Formulary for Children. There is no such thing as a universal ‘discard by’ date for suspensions - stability is determined by the manufacturer’s data and batch-specific testing. The suggestion that a parent can safely judge degradation by smell or color is not only unscientific but potentially hazardous. This is not advice - it is misinformation.
steve ker
January 22, 2026 AT 07:33lol why are we even talking about this. just give em pills. if they can't swallow then they're not sick enough to need antibiotics anyway. also i don't care if it's warm. it's medicine. it'll work. or it won't. whatever.