Getting a prescription wrong because of a missed or vague allergy note can be life-threatening. It’s not just a paperwork issue-it’s a safety issue. Every year in the U.S., drug allergies contribute to over 1.3 million injuries and 7,000 preventable deaths, according to the Institute of Medicine. The problem isn’t always the drug itself-it’s how poorly the allergy is documented in your medical records.
Why Vague Allergy Notes Are Dangerous
Many people say, “I’m allergic to penicillin,” or “I can’t take sulfa.” But those terms are too broad. Penicillin isn’t one drug-it’s a family. If you had a rash after taking amoxicillin, that’s not the same as being allergic to all penicillin-class antibiotics. And “sulfa” could mean sulfamethoxazole, sulfasalazine, or even a diuretic like furosemide. Confusing them leads to doctors avoiding safe, effective medications. A 2018 study at Massachusetts General Hospital found that 61% of patients had inaccurate or incomplete allergy records. Over 200 changes were made just by asking the right questions. One patient thought they were allergic to “ibuprofen” because they got a stomachache once. Turns out, they had a stomach virus that day. They were labeled allergic for 12 years-and missed out on pain relief that could’ve helped them.What Your Medical Record Needs to Include
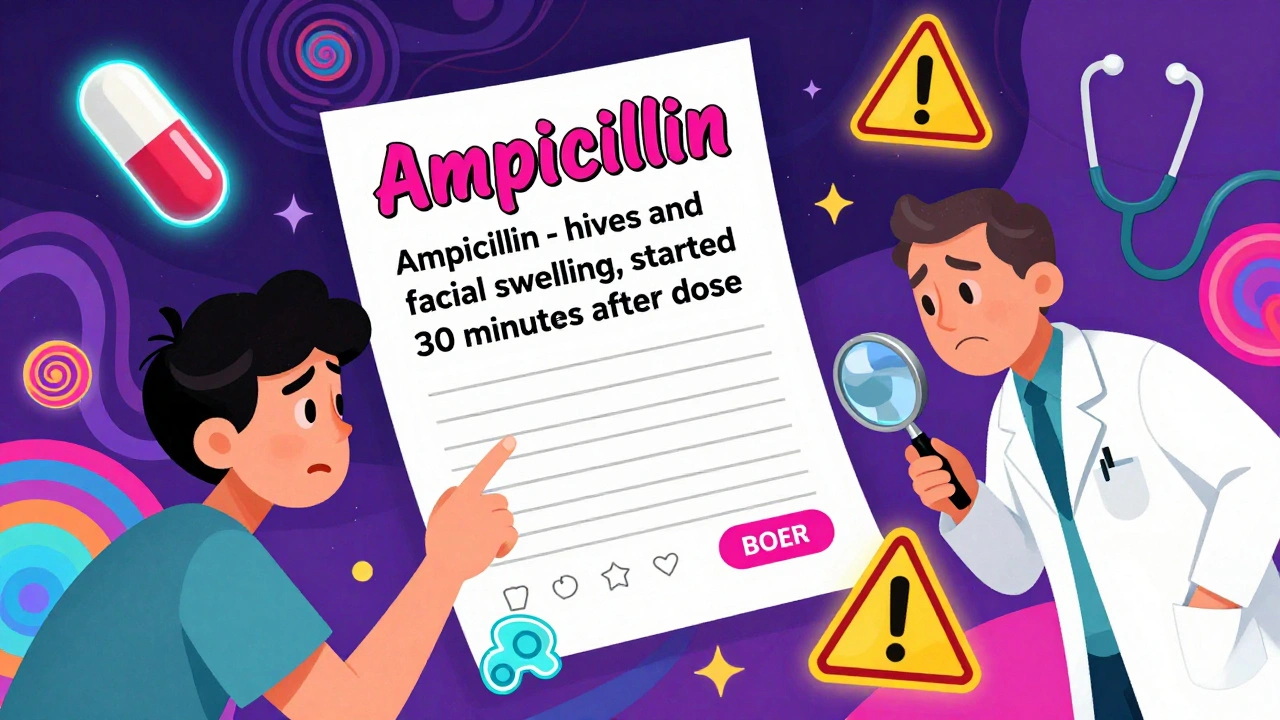
Your allergy entry isn’t complete if it just says “penicillin allergy.” Federal rules from the Centers for Medicare & Medicaid Services (CMS) require more. Every documented allergy must include:- The exact generic drug name (e.g., “ampicillin,” not “penicillin”)
- The signs and symptoms you experienced (rash, swelling, trouble breathing, vomiting, etc.)
- The severity of the reaction (mild, moderate, severe, life-threatening)
- The timing-how long after taking the drug did symptoms start?
How EHRs Are Built to Protect You
Most hospitals and clinics now use electronic health records like Epic, Cerner, or Meditech. These systems aren’t just digital charts-they’re safety nets. By 2014, CMS required all certified EHRs to:- Allow providers to record, edit, and access your active allergy list
- Require at least one allergy entry (or NKDA) for over 80% of patients
- Link allergies to clinical decision support tools that warn doctors before prescribing
What You Can Do to Keep Your Records Accurate
You’re not just a patient-you’re the most important part of your safety team. Here’s how to help:- Don’t guess. If you’re not sure what caused a reaction, say so. “I think it was the antibiotic” is better than “I’m allergic to antibiotics.”
- Bring your old records. If you’ve seen multiple doctors, bring printed copies or a list of past reactions. Many records get lost or merged incorrectly.
- Ask for a review. At your next appointment, say: “Can we go over my allergy list? I want to make sure it’s right.”
- Use the Drug Allergy History Tool. Some clinics now use this 10-minute questionnaire before appointments. It’s designed to uncover hidden or mislabeled allergies. Ask if it’s available.
- Know the difference between allergy and intolerance. Nausea, diarrhea, or headaches after a drug are usually side effects-not allergies. True allergies involve your immune system: hives, swelling, anaphylaxis, or trouble breathing.
What Happens If You Don’t Update Your Records
Outdated or vague allergy entries lead to real harm:- Doctors prescribe stronger, more expensive antibiotics you don’t need
- You get hospitalized for infections that could’ve been treated with simple pills
- You’re denied life-saving drugs during surgery or emergencies
- Emergency responders may avoid giving you epinephrine if they think you’re allergic to it (a common mistake)

Future Improvements Coming Soon
By 2025, the Office of the National Coordinator for Health IT plans to require EHRs to include patient-facing tools that let you update your own allergy list. You’ll be able to add reactions through a secure portal or app, and your doctor will get a notification. The FDA is also testing tools like MyStudies, which let patients report reactions directly from their phones. Early results show these tools capture more detail than doctor’s notes alone. Meanwhile, AI is being trained to scan free-text notes and pull out hidden allergy info. One study showed 85.7% accuracy in finding drug-reaction pairs buried in clinical summaries. That means even if you didn’t write it down clearly, the system might still catch it.Final Reminder: Accuracy Saves Lives
Your medical record isn’t just a file. It’s your shield. A poorly documented allergy can mean the difference between a quick recovery and a trip to the ICU. Don’t rely on memory. Don’t assume your doctor knows what you meant. Write it down clearly, review it regularly, and speak up if something doesn’t look right. Even small changes-like replacing “penicillin” with “amoxicillin” and adding “hives, 20 minutes after dose”-can help a doctor choose the right treatment the first time. That’s not just good documentation. That’s good medicine.What should I do if I think my drug allergy is listed wrong in my records?
Request a formal review of your allergy list during your next appointment. Bring a written account of your reaction, including the drug name, symptoms, timing, and severity. Ask your provider to update the record using the exact generic drug name and clear symptoms. If your clinic uses an EHR, request a printed copy of your current allergy list to verify accuracy.
Can I be allergic to a drug I’ve taken before without problems?
Yes. Drug allergies can develop at any time, even after multiple safe uses. Your immune system can change. If you experience new symptoms like hives, swelling, or breathing trouble after taking a medication you’ve used before, stop taking it and contact your doctor immediately. Update your record as soon as possible.
If I have a penicillin allergy, does that mean I can’t take any antibiotics?
No. Many people labeled with penicillin allergy can safely take other antibiotics. Only specific drugs in the penicillin family (like amoxicillin or ampicillin) are affected. Even then, many people who report penicillin allergy aren’t truly allergic-studies show 90-95% of them test negative. Ask your doctor about allergy testing to confirm whether you’re truly allergic.
Why do doctors ask about drug allergies every time I visit?
Because your allergy status can change. A reaction you had years ago might not be real, or you might have developed a new one. Federal guidelines require documentation to be reviewed at every admission or procedure-even if you’ve said “no allergies” before. This ensures your record is current and accurate when it matters most.
What if my doctor doesn’t update my allergy record correctly?
Politely insist on accuracy. Say: “I want to make sure this is documented correctly for my safety.” If they refuse or dismiss you, ask to speak with a patient advocate or medical records department. You have the right to request corrections under HIPAA. A vague or incorrect allergy entry puts you at risk, and you’re entitled to accurate records.
Kathleen Koopman
December 4, 2025 AT 14:38Shawna B
December 6, 2025 AT 13:55Jerry Ray
December 7, 2025 AT 09:25David Ross
December 8, 2025 AT 06:57Sophia Lyateva
December 9, 2025 AT 13:16Krys Freeman
December 10, 2025 AT 02:16Melania Dellavega
December 10, 2025 AT 08:31Bethany Hosier
December 11, 2025 AT 21:19AARON HERNANDEZ ZAVALA
December 13, 2025 AT 03:41