Hyponatremia Risk Assessment Tool
Risk Assessment Result
When sodium levels drop below normal, the heart has to work even harder. Hyponatremia is a condition where serum sodium concentration falls below 135mmol/L, often reflecting excess water relative to sodium. In patients with Heart Failurea chronic syndrome in which the heart cannot pump sufficient blood to meet the body’s needs, this electrolyte imbalance signals a worsening trajectory.
What Is Hyponatremia?
Hyponatremia can be hypovolemic (loss of both water and sodium), euvolemic (excess water with normal sodium), or hypervolemic (water overload with retained sodium). The hypervolemic form is most common in heart failure because the body mistakenly holds onto water to compensate for reduced cardiac output.
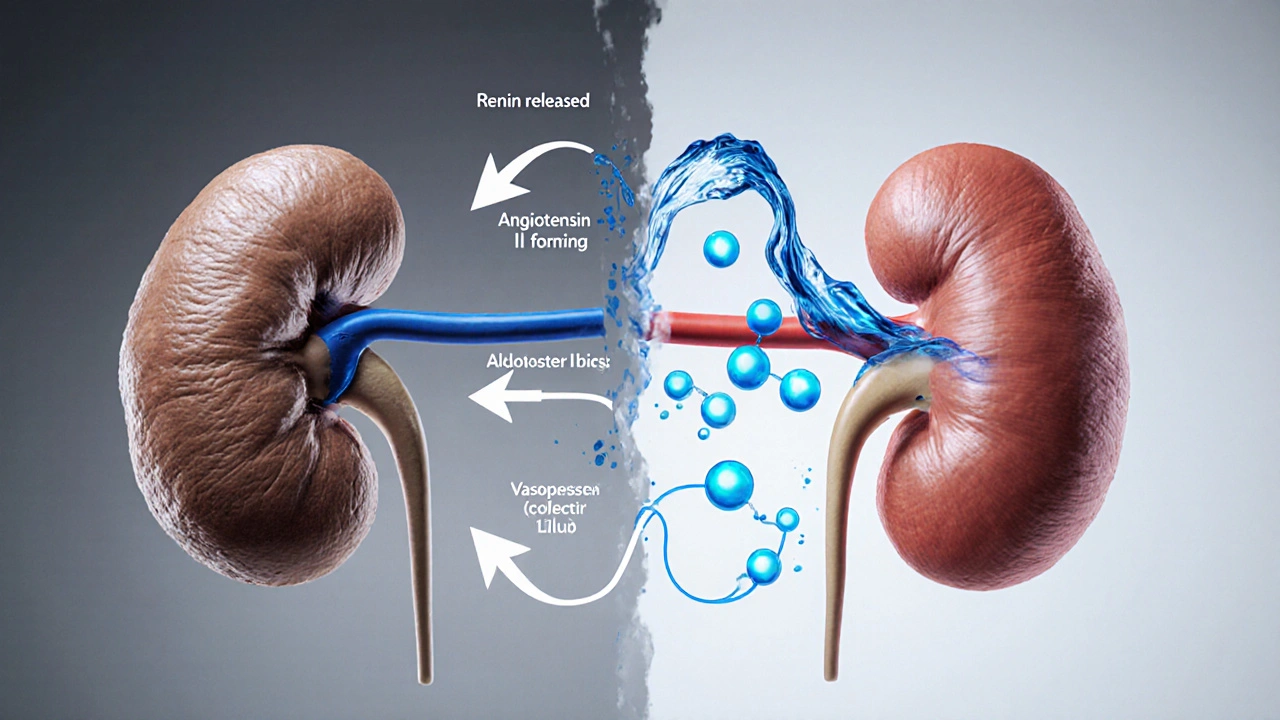
Key contributors include Renin‑angiotensin‑aldosterone systema hormonal cascade that tries to raise blood pressure by retaining sodium and water, and Vasopressinalso called antidiuretic hormone, it reduces urine output and traps free water. Both mechanisms become overactive as the heart struggles, leading to dilutional hyponatremia.
Heart Failure Basics
Heart failure is categorized by left‑ventricular ejection fraction: reduced EF (<40%) and preserved EF (≥50%). Regardless of type, patients experience elevated filling pressures, pulmonary congestion, and peripheral edema. The failing heart triggers neuro‑hormonal activation-again, RAAS and vasopressin-creating a vicious cycle of fluid retention.
Kidneysplay a central role in modulating blood volume by filtering plasma and reabsorbing sodium and water react to low perfusion by conserving sodium, yet paradoxically the body holds free water, diluting serum sodium.
How Low Sodium Worsens Heart Failure
The link isn’t just a lab curiosity; hyponatremia directly impacts cardiac performance. Low sodium reduces myocardial contractility, partly due to altered calcium handling inside heart cells. Moreover, a low serum sodium level is a surrogate marker for severe neuro‑hormonal activation, which drives further vasoconstriction and ventricular remodeling.
Clinical studies from the last decade consistently show that each 5mmol/L drop in sodium ups the risk of death by about 15% in chronic heart failure. The effect is independent of age, comorbidities, and even the use of guideline‑directed medical therapy.
Spotting Hyponatremia in Clinical Practice
Diagnosis starts with a basic chemistry panel. Serum Sodiummeasured in mmol/L, is the primary indicator. Values < 135mmol/L merit further work‑up; values < 130mmol/L often demand urgent intervention.
Additional clues include:
- Low plasma osmolality (< 275mOsm/kg)
- Elevated urinary sodium (> 20mmol/L) despite hyponatremia, suggesting inappropriate retention
- High brain natriuretic peptide (BNPa peptide released by stretched heart chambers, reflects volume overload) levels, which often accompany fluid overload
- Physical signs: peripheral edema, jugular venous distension, and pulmonary crackles
Importantly, rule out non‑cardiac causes- liver cirrhosis, SIADH, or certain medications-before attributing hyponatremia solely to heart failure.
Treatment Options: A Comparative Look
Management aims to raise serum sodium safely while relieving congestion. The table below breaks down the most common approaches.
| Strategy | Mechanism | Typical Sodium Rise (mmol/L/24h) | Key Risks | When to Use |
|---|---|---|---|---|
| Fluid Restriction (≤1.5L/day) | Limits free water intake, reduces dilution | 0-4 | Thirst, poor adherence | Mild‑to‑moderate hyponatremia, stable patients |
| Loop Diuretics (e.g., furosemide) | Inhibits Na‑K‑2Cl transporter, promotes natriuresis | 2-6 | Electrolyte loss, renal dysfunction | Volume overload with rising creatinine |
| Vaptans (e.g., tolvaptan) | Selective V2‑receptor antagonist, excretes free water | 4-8 | Over‑correction, liver toxicity | Severe euvolemic or hypervolemic hyponatremia, when diuretics fail |
| Hypertonic Saline (3% NaCl) | Directly raises serum sodium via osmotic gradient | 6-12 (rapid) | Osmotic demyelination if >10mmol/L rise in 24h | Life‑threatening hyponatremia (<125mmol/L) with neurologic symptoms |
Regardless of the chosen therapy, monitor sodium every 6-12hours during the first 48hours. Aim for a correction rate no faster than 8mmol/L in any 24‑hour period to avoid central pontine myelinolysis.

Prognosis: Why Sodium Levels Matter
Numerous registries-such as the ADHERE and OPTIMIZE‑HF studies-show that patients admitted with hyponatremia have longer hospital stays (average 7 vs 4days) and higher 30‑day readmission rates (35% vs 18%).
Beyond short‑term outcomes, low sodium predicts long‑term mortality. A meta‑analysis of 12 cohort studies found that a baseline sodium < 130mmol/L doubled the risk of death over a 5‑year follow‑up.
Importantly, correcting hyponatremia improves symptoms and may modestly lower mortality, but the benefit is greatest when treatment is combined with evidence‑based heart failure drugs (ARNI, beta‑blockers, mineralocorticoid receptor antagonists).
Practical Checklist for Clinicians
- Confirm hyponatremia with a repeat serum sodium.
- Assess volume status: look for edema, jugular venous pressure, lung crackles.
- Measure urinary sodium and osmolality to differentiate causes.
- Start with fluid restriction; add loop diuretics if congestion persists.
- Consider vaptans for refractory cases, but watch liver enzymes.
- If sodium < 125mmol/L or neurologic signs appear, begin hypertonic saline under ICU monitoring.
- Re‑measure sodium every 6-12hours; stop therapy if correction exceeds 8mmol/L/24h.
- Document discharge sodium and arrange early follow‑up (within 7days).
Frequently Asked Questions
What triggers hyponatremia in heart failure?
The failing heart reduces renal perfusion, which activates the renin‑angiotensin‑aldosterone system and vasopressin. These hormones cause the kidneys to retain water faster than sodium, diluting serum sodium.
How low does sodium have to be before I should treat?
Any value below 135mmol/L warrants evaluation. Urgent treatment is reserved for levels under 125mmol/L or when the patient shows confusion, seizures, or severe nausea.
Can I correct hyponatremia too quickly?
Yes. A rapid rise greater than 10mmol/L in 24hours can damage brain cells, leading to osmotic demyelination syndrome. Stick to a correction ceiling of 8mmol/L per day.
Do vaptans replace diuretics?
No. Vaptans are useful when diuretics fail to raise sodium or cause worsening renal function. They are usually added to, not substituted for, loop diuretics.
Will fixing sodium improve survival?
Correcting sodium improves symptoms and reduces readmissions. Survival benefits appear when correction is part of a comprehensive heart‑failure regimen, not when done in isolation.
tabatha rohn
October 10, 2025 AT 21:28Hyponatremia is just a lazy excuse for doctors who can’t manage fluids 😒
Mark Rohde
October 15, 2025 AT 15:09Look at the hype around vaptans – it’s pure drama 🚩 they’re not the silver bullet and the side‑effects are scary 😬
Rajan Desai
October 20, 2025 AT 08:50The renin‑angiotensin‑aldosterone system ramps up in heart failure to retain sodium, but paradoxically water retention dominates because vasopressin spikes, diluting serum sodium. As cardiac output falls, baroreceptors trigger ADH release, which reduces free water excretion. This creates a hypervolemic hyponatremia that signals worsening congestion. Clinically, you’ll see low serum osmolality alongside elevated BNP. Correcting the sodium too fast can cause osmotic demyelination, so gradual adjustment is key.
S O'Donnell
October 25, 2025 AT 02:31While the preceding explanation captures the essential physiology, it neglects several critical nuances that a true connoisseur of heart failure management would never overlook.
First, the interplay between atrial natriuretic peptide and vasopressin is a bidirectional feedback loop, not merely a one‑way street.
Second, the renal handling of sodium in the setting of loop diuretic resistance involves compensatory upregulation of the sodium‑hydrogen exchanger in the distal tubule.
Third, chronic activation of the sympathetic nervous system further impairs renal perfusion, exacerbating the tendency toward water retention.
Moreover, the concept of “dilutional hyponatremia” is overly simplistic, as intracellular shifts of osmolytes can also contribute to serum sodium decline.
In practice, clinicians should monitor urine osmolality in addition to serum sodium to gauge the effectiveness of ADH blockade.
The use of tolvaptan, while promising, requires vigilant serum sodium checks every 6‑8 hours to avoid overshoot.
Hypertonic saline, though effective for rapid correction, demands concurrent loop diuretic therapy to prevent volume overload.
Additionally, dietary sodium restriction below 2 g per day can paradoxically worsen neurohormonal activation if not paired with appropriate diuresis.
Emerging data also suggests that SGLT2 inhibitors may modestly improve free water clearance by enhancing osmotic diuresis.
Finally, the prognostic value of hyponatremia extends beyond fluid status; it is an independent predictor of mortality even after adjusting for ejection fraction.
Thus, treating hyponatremia is not merely about correcting a lab value but about attenuating the maladaptive neurohormonal cascade.
In sum, a comprehensive approach that integrates diuretic sequencing, ADH antagonism, and meticulous electrolyte monitoring is indispensable.
Neglecting any of these components can precipitate rapid shifts in serum sodium, placing patients at risk for osmotic demyelination syndrome.
Hence, the clinician’s toolbox must be both broad and precise to navigate the delicate balance of fluid and electrolyte homeostasis in heart failure.
Yamunanagar Hulchul
October 29, 2025 AT 19:12Wow, what a fantastic reminder that early sodium monitoring can actually save lives!!! 🎉 Keeping an eye on those numbers, staying hydrated wisely, and adjusting meds promptly make a huge difference in patient outcomes!!! 🌟
Sangeeta Birdi
November 3, 2025 AT 12:53Absolutely, staying proactive with labs feels like giving patients a safety net, and the extra smile 🙂 you get from them when they improve is priceless.
Chelsea Caterer
November 8, 2025 AT 06:35Salt is the silent whisper of the heart’s struggle.
Adam Dicker
November 13, 2025 AT 00:16Let’s get out there and tackle hyponatremia head‑on! With the right diuretic plan and vigilant labs, we can turn a worsening picture into a success story. Keep pushing forward, team!
Molly Beardall
November 17, 2025 AT 17:57Sure, but the “success story” narrative ignores the ugly reality of over‑correction risks – you can’t just gloss over osmotic demyelination.
Brian Pellot
November 22, 2025 AT 11:38Valid point – balance is key. Guideline‑driven protocols help us stay safe while still being aggressive enough to improve symptoms.
Patrick McCarthy
November 27, 2025 AT 05:19BNP spikes often line up with dropping sodium levels showing how congestion drives hyponatremia
Henry Seaton
December 1, 2025 AT 23:00American guidelines are the gold standard for hyponatremia management.
Amy Hamilton
December 6, 2025 AT 16:41From a global perspective, embracing diverse treatment strategies enriches our collective knowledge; when we share successes across borders, patient care flourishes. Let’s celebrate the collaborative spirit that drives innovation in heart failure therapy!
Lewis Lambert
December 11, 2025 AT 10:22One of the most under‑appreciated tools is bedside ultrasound to assess IVC diameter – it gives real‑time insight into volume status, guiding diuretic intensity and preventing unnecessary fluid restriction.
Tamara de Vries
December 16, 2025 AT 04:03Take it step by step, listen to your patients, and trust the gradual improvements – you’ll get there.
Jordan Schwartz
December 20, 2025 AT 21:44Balancing fluid restriction with quality of life is a nuanced dance, but with careful monitoring and patient education, most can achieve stable sodium without feeling overly thirsty.
Dawn Midnight
December 25, 2025 AT 15:25Just a quick note: “hypervolemic” should be hyphenated as “hyper‑volemic” when used as an adjective before a noun, and “BNP” is an acronym that doesn’t need an article.
frank hofman
December 30, 2025 AT 09:06Honestly, all that fancy tech sounds cool but most clinics still get by just using plain old weight checks 😅
Dannii Willis
January 4, 2026 AT 02:47Interesting thread, learned a few new tips today.
Robyn Du Plooy
January 8, 2026 AT 20:28The interplay of neurohormonal activation, aquaresis via V2‑receptor antagonism, and diuretic sequencing embodies the quintessential cardio‑renal nexus that defines modern heart failure therapeutics.