COPD & Anxiety Symptom Tracker
Track Your COPD Symptoms
Shortness of Breath
Anxiety Level
Track Your Breathing Exercises
Your Tracking History
No entries yet. Start tracking your symptoms to see patterns.
Did you know that up to 40% of people living with chronic obstructive pulmonary disease (COPD) also battle significant anxiety? That overlap isn’t a coincidence - the two conditions feed each other in a vicious cycle.
Quick Takeaways
- Breathlessness triggers the body's stress response, raising cortisol and heart rate.
- Fear of an attack can turn normal activities into sources of dread.
- Effective management blends respiratory treatment with proven anxiety‑reduction techniques.
- Early mental‑health screening improves quality of life and reduces hospital admissions.
What Is COPD?
Chronic Obstructive Pulmonary Disease is a progressive lung disorder characterized by narrowed airways, chronic inflammation, and irreversible damage to the alveoli. It typically develops after decades of exposure to irritants-most commonly cigarette smoke-but can also result from air‑pollution, occupational dust, or genetic factors such as alpha‑1 antitrypsin deficiency.
The hallmark symptoms are persistent cough, sputum production, and, crucially, dyspnea-or shortness of breath-that worsens with activity. Advanced COPD reduces the lungs' ability to exchange oxygen and carbon dioxide, leading to chronic hypoxia.

What Is Anxiety?
Anxiety is a mental‑health condition marked by excessive worry, tension, and physical symptoms like rapid heartbeat, trembling, and shortness of breath. While occasional nervousness is normal, clinical anxiety persists, interferes with daily life, and can manifest as panic attacks, generalized anxiety disorder (GAD), or specific phobias.
In the context of chronic illness, anxiety often stems from fear of symptom escalation, loss of independence, or uncertainty about the future.
Why Breathlessness Sparks Anxiety
The sensation of not getting enough air is one of the most primal threats our bodies recognize. When a COPD patient experiences breathlessness, the brain’s amygdala lights up the same circuitry that triggers a "fight‑or‑flight" response.
The cascade looks like this:
- Reduced airflow → low oxygen (hypoxia) and high carbon dioxide.
- Hypoxia stimulates the sympathetic nervous system.
- Adrenal glands release cortisol and adrenaline.
- Heart rate, muscle tension, and hyperventilation increase, mimicking panic.
Because the body interprets these physical cues as danger, even a mild episode can spiral into full‑blown anxiety.
Psychological Impact of Living with COPD
Beyond the immediate physiological loop, chronic breathlessness reshapes a person’s outlook:
- Activity avoidance: Fear of becoming winded leads patients to skip walks, social events, or chores, which in turn reduces fitness and worsens lung function.
- Social isolation: Exhaustion and embarrassment about coughing or sputum can drive people away from friends and family.
- Loss of control: COPD’s unpredictable flare‑ups create a sense of helplessness, a known catalyst for anxiety and depression.
Research from the British Thoracic Society (2023) showed that patients who reported high anxiety scores were 1.7times more likely to be hospitalized for COPD exacerbations within the next year.
Managing Anxiety When You Have COPD
Effective care requires a two‑pronged approach: treat the lungs *and* calm the nervous system.
1. Optimize Respiratory Therapy
Good control of COPD symptoms reduces the physiological triggers of anxiety.
- Bronchodilators: Short‑acting (e.g., albuterol) for rescue, long‑acting (e.g., tiotropium) for maintenance.
- Inhaled corticosteroids: Lower airway inflammation, especially for patients with frequent exacerbations.
- Pulmonary rehabilitation: A structured program of exercise, education, and breathing techniques that improves lung capacity and confidence.
Pulmonary rehabilitation has been shown to cut anxiety scores by an average of 12 points on the Hospital Anxiety and Depression Scale (HADS) after eight weeks.
2. Breath‑Control Techniques
Learning how to breathe efficiently can break the panic loop.
- Pursed‑lip breathing: Inhale through the nose, exhale slowly through pursed lips, extending the exhalation phase to keep airways open.
- Diaphragmatic breathing: Focus on expanding the belly rather than the chest; this reduces the work of breathing and calms the autonomic nervous system.
- Box breathing (4‑4‑4‑4 seconds): Often used by athletes and military personnel to reset heart rate.
Practice these techniques twice daily and during flare‑ups for best results.
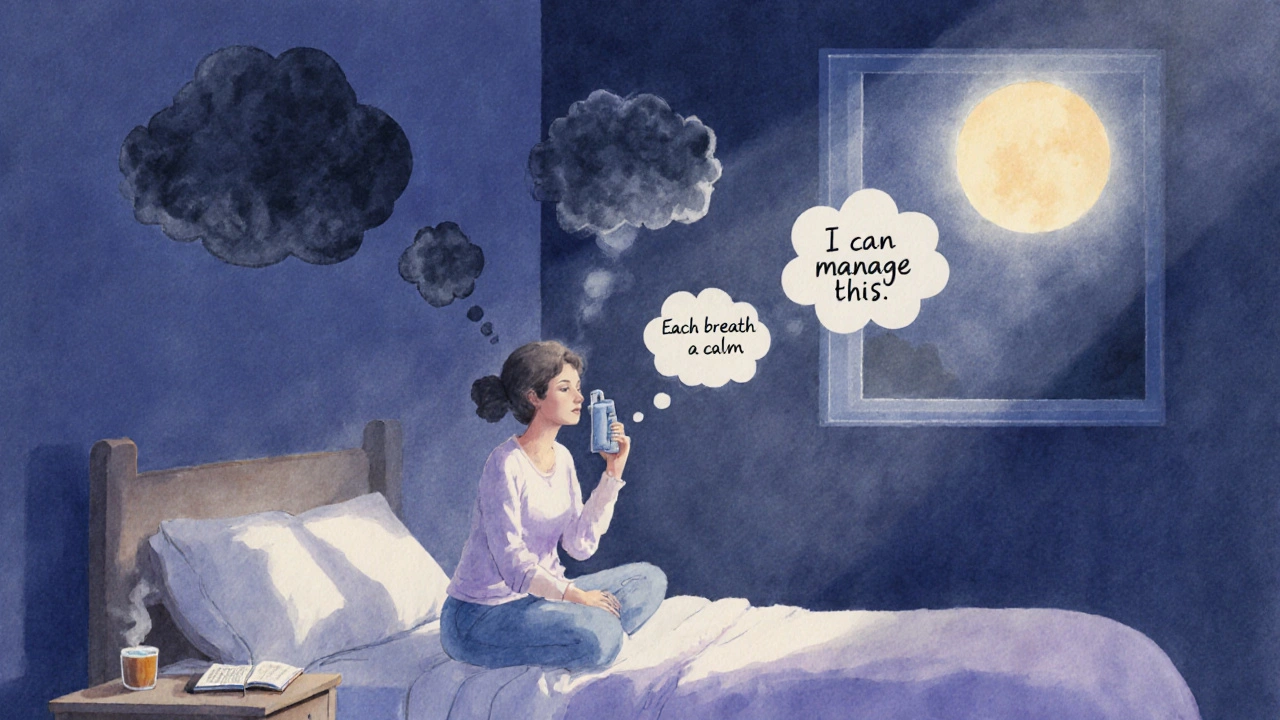
3. Cognitive‑Behavioral Strategies
CBT helps reframe catastrophic thoughts that arise when shortness of breath strikes.
- Identify automatic thoughts like "If I can’t breathe, I’ll die".
- Challenge them with evidence (e.g., "I have rescue inhaler that works in minutes").
- Replace with realistic statements such as "I can manage this with my breathing tools".
Many community health clinics in the UK now offer CBT groups specifically for chronic‑illness patients.
4. Lifestyle Adjustments
- Quit smoking (if applicable): Smoking fuels both COPD progression and anxiety by irritating the airways and raising cortisol.
- Regular low‑intensity activity: Walking, swimming, or stationary cycling improves aerobic capacity without overtaxing the lungs.
- Mind‑body practices: Yoga, tai chi, and guided meditation have been linked to lower HADS scores in COPD cohorts.
5. When to Seek Professional Help
If anxiety interferes with medication adherence, sleep, or daily functioning, a referral to a mental‑health specialist is warranted. Pharmacologic options-such as low‑dose selective serotonin reuptake inhibitors (SSRIs)-can be safely combined with COPD treatments under medical supervision.
Putting It All Together: A Sample Day Plan
- Morning: 5‑minute pursed‑lip breathing, short walk (5‑10min) with inhaler on hand.
- Mid‑day: Lunch with a friend; practice mindful eating to stay present and reduce worry.
- Afternoon: Attend pulmonary rehab class (includes exercise, breathing drills, group discussion).
- Evening: 10‑minute diaphragmatic breathing before bed, jot down any anxious thoughts, reframe them using CBT worksheets.
Consistency is key-small daily actions prevent the anxiety spiral from gaining momentum.
Frequently Asked Questions
Can anxiety make COPD symptoms worse?
Yes. Anxiety triggers the sympathetic nervous system, increasing heart rate and airway constriction, which can intensify dyspnea and lead to more frequent flare‑ups.
Is it safe to take anti‑anxiety medication with inhalers?
Generally, yes. SSRIs and low‑dose benzodiazepines do not interfere with bronchodilators. Always discuss dosage and potential interactions with your GP or respiratory specialist.
How often should I practice breathing exercises?
Aim for at least two structured sessions per day-once in the morning and once before bed. During an exacerbation, use them as often as needed to calm panic.
What role does smoking cessation play in anxiety reduction?
Quitting smoking removes a major irritant that worsens both COPD and cortisol spikes. Many ex‑smokers report a noticeable drop in anxiety levels within the first three months of abstinence.
Are there any non‑pharmacologic programs specifically for COPD‑related anxiety?
Yes. Several NHS trusts run combined pulmonary‑rehabilitation and CBT workshops. These programs teach breathing control, relaxation, and cognitive‑reframing in a supportive group setting.

Brandi Hagen
October 8, 2025 AT 13:38Let me tell you, the relationship between COPD and anxiety is a perfect storm that can turn everyday life into a relentless nightmare, especially when you consider the physiological cascade that starts with that terrifying feeling of not getting enough air! 😱 The brain’s amygdala lights up like a fireworks display, flooding the body with cortisol and adrenaline, which only makes the lungs work harder and the heart pound faster. 🌪️ Every gasp for breath becomes a reminder of mortality, and before you know it, a simple walk to the mailbox feels like scaling a mountain. 🏔️ The fear of an exacerbation is not just in your head; it’s wired into your nervous system, creating a feedback loop that amplifies both breathlessness and dread. 🚨 Studies show that up to 40% of COPD patients also wrestle with significant anxiety, and that’s not a coincidence – it’s a biological reality. 📊 When you add the stigma of using inhalers in public, the social isolation kicks in, further feeding the anxious thoughts. 😔 This isolation can lead to reduced physical activity, which then worsens lung function, making any future breathlessness even more terrifying. 🎭 The drama doesn’t end there; anxiety can cause hyperventilation, which reduces CO₂ levels and triggers panic attacks, making the whole cycle look like a vicious, endless loop. 🔄 Imagine trying to focus on work while your chest feels like it’s under a vice – productivity plummets, and stress skyrockets. 📉 The good news is that there are evidence‑based strategies to break this chain, from pulmonary rehabilitation to cognitive‑behavioral therapy, each targeting a different rung of the ladder. 🛠️ Breathing exercises like pursed‑lip and diaphragmatic breathing can calm the nervous system, while regular low‑intensity activity rebuilds confidence in your body’s capabilities. 🏃♀️ And let’s not forget the power of a supportive community – sharing experiences can diminish that feeling of being alone in the struggle. 🤝 So, if you’re battling COPD, remember that managing anxiety isn’t a side quest; it’s a core part of the treatment plan that can dramatically improve quality of life. 🌟 Keep tracking your symptoms, stay consistent with your breathing drills, and don’t shy away from seeking mental‑health support – the battle is tough, but you’re tougher! 💪
isabel zurutuza
October 8, 2025 AT 13:56Oh great another guide on breathing, exactly what my coffee needed today
James Madrid
October 8, 2025 AT 14:13Hey folks, just wanted to add a quick note of encouragement. If you’re dealing with both COPD and anxiety, remember that small, consistent steps can lead to big improvements. Start with a few minutes of pursed‑lip breathing each morning – it’s low‑effort but high‑impact. Pair that with a short walk, even just around the block, and you’ll notice a boost in confidence. Don’t underestimate the power of tracking your symptoms; seeing patterns can empower you to act before things spiral. And if you ever feel overwhelmed, reach out to a respiratory therapist or a counselor – they’re there to help you succeed. Keep at it, you’ve got this!
Justin Valois
October 8, 2025 AT 14:30Alright, let me break it down for the clueless masses. COPD ain’t just a cough, it’s a full‑blown siege on your lungs that makes your brain think you’re drowning every time you huff and puff. Then you add anxiety to the mix and boom – you’ve got a perfect recipe for panic attacks that feel like the world’s ending. The amygdala lights up like a fireworks show at 4th of July and you start hyperventilating, which just makes the oxygen shortage worse. People love to act like it’s all in your head, but the science says otherwise, so stop the nonsense. Also, stop ignoring those inhalers you got – they’re not just decorative. And for the love of all that’s holy, quit smoking, because that damn habit just fuels the whole disaster. If you want real results, join a pulmonary rehab program, do the breathing drills they teach, and actually practice them – no half‑assing it. Trust me, you’ll see a drop in those anxiety scores if you actually give a damn about the process.
Jessica Simpson
October 8, 2025 AT 14:46It’s fascinating how respiratory health intertwines with mental wellbeing across cultures. In many Indigenous communities, breathing practices are woven into daily rituals, offering both physical relief and spiritual grounding. Incorporating such holistic approaches alongside conventional therapies could enrich the management of COPD‑related anxiety. Exploring these cultural perspectives can provide fresh insights for practitioners and patients alike.
Ryan Smith
October 8, 2025 AT 15:03Funny how the pharma giants push inhalers while the real cause of our breathlessness is the silent chemtrails above us. 😒 They want us dependent, scared, and too busy worrying about our lungs to question the bigger picture. So when they tell you to take an SSRI, just remember it’s another chip in the system. Stay vigilant, keep your mind clear, and don’t let them dictate your breathing.
John Carruth
October 8, 2025 AT 15:20First off, great job laying out the science – it’s clear that the mind‑body connection is real and powerful. I’d like to add a bit of practical advice for anyone reading this. Start each day with a 5‑minute session of diaphragmatic breathing; place a hand on your belly and focus on expanding it with each inhale. Follow that with a quick stretch, like raising your arms overhead to open the chest cavity. Then, take a short walk outside, even if it’s just to the end of the driveway, and practice pursed‑lip breathing if you feel short of breath. This routine helps reset the nervous system and can reduce the “fight‑or‑flight” response that anxiety triggers. Also, consider keeping a simple log – write down the time you exercised, the breathing technique used, and a quick note on how you felt afterward. Over weeks, you’ll see patterns that empower you to adjust your plan. Remember, consistency beats intensity every time. Keep at it, and you’ll likely notice fewer panic spikes and a steadier lung performance. You’ve got this, and the community is here to cheer you on!
Melodi Young
October 8, 2025 AT 15:36Nice info, but let’s be real – most people don’t have the time or energy to log every breath and anxiety spike. The system’s already demanding enough without adding a spreadsheet. Still, kudos for the thoroughness, just wish it was a bit more practical for everyday folks.
Tanna Dunlap
October 8, 2025 AT 15:53The moral of the story is that neglecting mental health while battling a chronic disease is simply irresponsible. Society tends to glorify stoicism, but failing to address anxiety in COPD patients only amplifies suffering and healthcare costs. It’s high time we demand integrated care models that treat the whole person, not just the lungs.
Troy Freund
October 8, 2025 AT 16:10When you think about it, breathing is the most literal form of presence – each inhale anchors us to the here and now, each exhale releases the weight of yesterday. Embracing that philosophy can turn a simple breathing exercise into a meditation on existence, easing both physical and mental strain. So, make each breath count, not just for oxygen, but for the quiet moments it gifts us.
Mauricio Banvard
October 8, 2025 AT 16:26Alright, let’s cut the fluff. The data is clear: COPD + anxiety = higher hospital readmission rates. If you want to avoid becoming a statistic, grab your inhaler, do the breathing drills, and stop procrastinating on that therapy appointment. No more excuses, no more doom‑and‑gloom – just action.