What Is a Hip Labral Tear?
A hip labral tear happens when the ring of cartilage around the socket of your hip joint gets damaged. This cartilage, called the labrum, acts like a gasket-it keeps the ball of your femur snug in the socket and helps absorb shock during movement. When it tears, you don’t just feel a dull ache. You get sharp pain in the groin, clicking or locking in the hip, and stiffness that makes even walking uncomfortable. For athletes, this isn’t just an inconvenience-it can end a season or derail a career.
It’s not random. Most tears come from femoroacetabular impingement (FAI), where bone growths on the hip joint rub against the labrum over time. Think of it like a misaligned door hinge that grinds itself apart. Basketball players, soccer midfielders, hockey defensemen, and distance runners are at highest risk because their hips are constantly twisting, flexing, and rotating under load. Studies show 22% to 55% of athletic hip pain cases involve a labral tear, especially in athletes under 40.
Why Imaging Matters-MRA Is the Gold Standard
Many athletes get an X-ray first. That’s fine for spotting bone spurs or hip dysplasia, but X-rays won’t show the labrum. Standard MRI helps, but it misses up to 30% of partial tears. That’s why magnetic resonance arthrography (MRA) is the go-to test. In MRA, contrast dye is injected into the hip joint before the scan. This dye highlights the labrum like ink in a blueprint, making even tiny frays visible. Studies confirm MRA detects labral tears with 90-95% accuracy, compared to just 35-60% for regular MRI.
Doctors also look for other red flags during imaging: synovitis (inflamed joint lining), loose fragments floating in the joint, or signs of early arthritis. These aren’t side notes-they change the game. If you have a labral tear plus hip dysplasia (a shallow socket), treating just the tear won’t fix the problem. The socket needs to be reshaped too, or the tear will come back. That’s why 3D MRI sequences, now recommended by the International Hip Arthroscopy Society, are becoming standard for complex cases. They give surgeons a full 360-degree view before they even cut into the joint.
Physical Tests That Reveal the Tear
Before imaging, your doctor will move your hip in specific ways. Two tests are most telling: FADIR and FABER. FADIR means bending your knee to 90 degrees, pulling it toward your chest, then pushing it inward. If that triggers sharp groin pain, it’s a strong sign of a labral tear. FABER-flexing, abducting, and externally rotating the hip-can reproduce a clicking sensation or deep ache. These tests are accurate in 78% of confirmed cases. No fancy machine needed. Just skilled hands and a clear understanding of how the hip moves.
But here’s the catch: other conditions mimic labral tears. Athletic pubalgia, piriformis syndrome, bursitis, even osteoarthritis can feel the same. That’s why a full exam matters. If you’ve been told you have “hip bursitis” for months and nothing’s changed, ask for an MRA. Many athletes waste months on wrong diagnoses because the pain pattern overlaps. Don’t let that be you.

Conservative Treatment: When It Works (and When It Doesn’t)
Not every labral tear needs surgery. For mild cases, doctors start with rest, anti-inflammatories like ibuprofen or naproxen, and avoiding movements that aggravate the hip. Physical therapy is controversial-some studies say only 30-40% of athletes recover fully without surgery. But clinics like True Sports Physical Therapy report 65% success with tailored rehab programs. The difference? Customized plans. Generic stretching won’t cut it. You need exercises that strengthen the glutes, stabilize the pelvis, and improve hip mobility without overloading the labrum.
Corticosteroid injections can buy time. They reduce inflammation and give 70-80% of patients relief for 3-6 months. That’s useful if you’re trying to finish a season or delay surgery. But injections don’t heal the tear. They just mask the pain. If you rely on them long-term, you risk doing more damage without realizing it.
The real problem? Insurance. MRA costs $1,200-$1,800 out-of-pocket. Standard MRI is half that. Many athletes skip the best test because they can’t afford it. That’s why some end up with misdiagnoses and delayed treatment. If you’re an athlete and your hip pain won’t go away, push for the right imaging. Your future self will thank you.
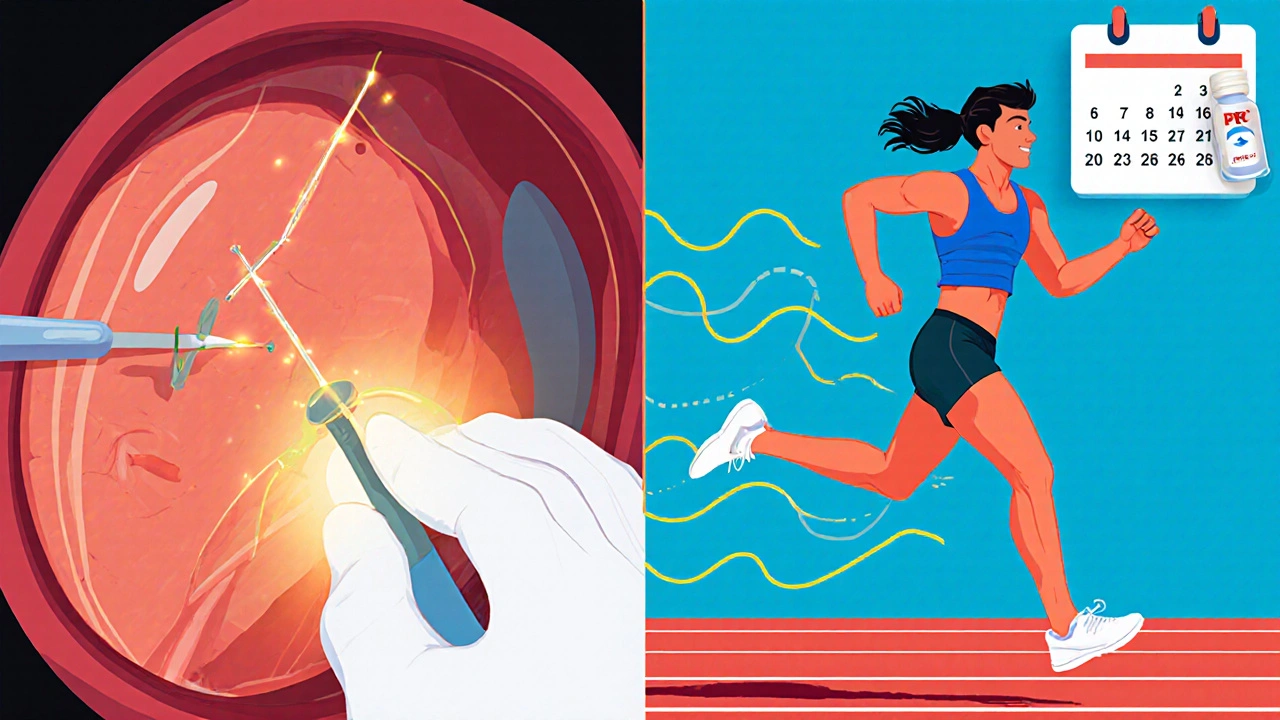
Arthroscopy: The Procedure That Changes Everything
If conservative care fails after 3-6 months, arthroscopy is the next step. It’s minimally invasive. Two small incisions, a camera, and tiny instruments. The surgeon looks directly at the labrum-98% accurate, no guesswork. Then comes the decision: repair or remove?
Repair means stitching the torn labrum back to the bone with suture anchors. This is preferred when the tissue is still healthy. Debridement means trimming away the frayed edges. It’s quicker, but it doesn’t fix the root problem. The American Academy of Orthopaedic Surgeons warns: if you have FAI or hip dysplasia and only do debridement, you’re 40% more likely to need revision surgery later.
That’s why modern surgery isn’t just about the labrum. If your hip shape is abnormal, the surgeon will reshape the bone at the same time. This is called osteoplasty. It’s not optional in many cases-it’s essential. A 2023 study showed isolated labral repair in dysplastic hips fails in 65% of cases within two years. Fix the structure, fix the tear.
Recovery: What Athletes Really Experience
Recovery isn’t the same for everyone. It depends on the procedure, your sport, and how well you stick to rehab.
- Debridement: 3-4 months to return to sport. Less pain, faster return, but higher risk of re-injury if the root cause isn’t fixed.
- Labral repair: 5-6 months. You can’t rush this. The stitched labrum needs time to heal into the bone. Most protocols require 12 weeks of physical therapy before even starting sport-specific drills.
Success hinges on three things: achieving 90% quadriceps strength symmetry, pain-free internal rotation to at least 30 degrees, and no swelling after activity. If you’re a runner, you can’t just start jogging again. You need to rebuild stride mechanics. A dancer? You need to retrain rotation without stressing the hip.
Real stories vary. One marathon runner returned at 4.5 months with strict rehab. A professional hockey player took 5.5 months. But a competitive dancer had to get revision surgery because her first surgeon didn’t spot the underlying FAI. The difference? Access to specialized care. Athletes treated at dedicated sports medicine centers report 92% satisfaction. At general orthopedic clinics? Only 75%.
New Tech and Future Trends
The field is moving fast. In June 2023, the FDA approved Smith & Nephew’s BioX-a bioabsorbable suture anchor that dissolves over time. Early data shows 89% success at two years, better than traditional metal anchors. That’s a big deal. No more permanent hardware in your hip.
Regenerative medicine is also gaining ground. Platelet-rich plasma (PRP) injections, where your own blood is concentrated and injected into the hip, helped 55% of patients avoid surgery in a 2022 trial. It’s not a cure-all, but for some, it’s a bridge.
By 2027, experts predict 75% of labral repairs will be done entirely through arthroscopy-no open surgery needed. And the market? It’s growing. Over 150,000 hip arthroscopies were done in the U.S. in 2022, up 300% since 2010. More athletes are getting diagnosed, and more surgeons are trained to fix them.
What Happens If You Do Nothing?
Ignoring a labral tear isn’t an option. A 15-year study found untreated tears lead to a 4.5 times higher risk of developing hip osteoarthritis within a decade. The labrum isn’t just padding-it’s a shock absorber. When it’s gone, bone grinds on bone. That’s permanent. And once arthritis sets in, your options shrink. You might end up needing a hip replacement in your 40s or 50s.
This isn’t just about pain. It’s about preserving your ability to move, play, and live without limits. For athletes, that’s everything.
Final Thoughts: Know Your Options
A hip labral tear isn’t a death sentence. It’s a signal. It tells you something’s off in your joint mechanics. The best outcome comes from early, accurate diagnosis-MRA over standard MRI-and treatment that addresses the whole problem, not just the tear. Whether you choose rehab or surgery, the key is working with a team that understands athletic hips. Don’t settle for a quick fix. Your body is your tool. Protect it like one.
Can a hip labral tear heal without surgery?
Yes, but only in mild cases. If the tear is small and there’s no underlying bone abnormality like FAI or hip dysplasia, rest, physical therapy, and activity modification can reduce symptoms. However, studies show only 30-65% of athletes achieve full recovery without surgery. For most competitive athletes, especially those with structural issues, surgery offers better long-term outcomes.
Is MRA really necessary, or is a regular MRI enough?
MRA is far more accurate. Standard MRI misses up to 30% of labral tears, especially partial ones. MRA uses contrast dye injected into the joint, making the labrum stand out clearly. With 90-95% sensitivity, it’s the gold standard for diagnosis. If your pain persists and your MRI was normal, push for an MRA. A missed tear can lead to worse damage down the line.
How long does recovery take after hip arthroscopy?
Recovery depends on the procedure. Debridement usually takes 3-4 months. Labral repair takes 5-6 months because the tissue needs to reattach to bone. Full return to sport requires passing strength and mobility tests-like 90% quadriceps symmetry and pain-free internal rotation. Rushing back increases the risk of re-tear. Most athletes need 6 months of structured rehab before returning to high-impact sports.
Do I need surgery if I have hip dysplasia and a labral tear?
Yes. If you have hip dysplasia (a shallow socket), repairing just the labrum isn’t enough. The socket needs to be surgically reshaped to prevent the labrum from tearing again. Studies show isolated labral repair in dysplastic hips fails in 65% of cases within two years. Correcting the bone structure along with the tear is critical for long-term success.
What sports carry the highest risk for hip labral tears?
Sports with repetitive hip rotation and deep flexion carry the highest risk. Basketball (22%), soccer (18%), hockey (15%), and running (12%) top the list. Ballet, gymnastics, and martial arts also place extreme stress on the hip joint. Athletes in these sports often develop FAI over time, which leads to labral damage. Prevention includes mobility work, core strength, and avoiding overtraining.
Are there alternatives to surgery for hip labral tears?
Yes, but they’re not always effective long-term. Conservative options include rest, NSAIDs, corticosteroid injections, and physical therapy. PRP injections have shown promise in 55% of cases, helping some avoid surgery. However, if there’s structural damage like FAI or dysplasia, these methods won’t stop the tear from worsening. Surgery remains the only way to address the root cause in most athletic cases.

Srikanth BH
November 24, 2025 AT 15:34Been through this myself after a soccer injury. MRA saved my season-regular MRI said 'nothing serious.' Turns out I had a partial tear plus FAI. Took 6 months to come back, but now I’m running again without pain. Don’t skip the dye.
Josh Gonzales
November 26, 2025 AT 04:15Why do so many docs still start with X-rays when MRA is clearly superior? It’s like checking the tire pressure with a ruler. Also, PRP isn’t magic but it’s cheaper than surgery and worth a shot if you’re not elite level
Valérie Siébert
November 27, 2025 AT 02:01OMG YES I’M A DANCER AND MY SURGEON DIDN’T EVEN LOOK FOR FAI FIRST. I GOT DEBRIDEMENT AND 8 MONTHS LATER I WAS BACK IN PHYSICAL THERAPY BECAUSE IT TORE AGAIN. WHY DO PEOPLE DO THIS TO US. I’M STILL ANGRY. 2023. WE HAVE 3D IMAGING. FIX THE STRUCTURE OR DON’T OPERATE AT ALL.
Jack Riley
November 27, 2025 AT 19:14It’s funny how we treat the hip like a disposable part. We run, twist, squat, and then act shocked when it breaks. The body’s not a machine you can upgrade-it’s a living ecosystem. A labral tear isn’t just a torn cartilage, it’s your joint screaming that you’ve been treating it like a prop, not a partner. You don’t fix a tear with stitches alone-you fix the movement patterns that caused it. And yet, most rehab programs still focus on glute bridges like it’s 2010. We’re still treating symptoms, not the metaphysics of motion.
And let’s talk about insurance. You’re telling me a $1,500 scan is too expensive but a $40,000 surgery is fine? That’s not healthcare, that’s capitalism with a stethoscope. If you can’t afford the diagnosis, you’re just gambling with your future mobility. And guess who pays? The future you. The one who can’t climb stairs without wincing at 42.
PRP? Cute. It’s like putting duct tape on a cracked engine block. It might quiet the noise for a while, but the metal’s still fatiguing. And those bioabsorbable anchors? Finally. We’re moving from ‘screw it in and forget’ to ‘let the body rebuild.’ That’s evolution. Not revolution. Evolution.
And the athletes who skip rehab? You’re not brave. You’re just impatient. Healing isn’t a countdown. It’s a conversation between tissue and time. You don’t sprint back into a game because your pain is gone. You sprint back when your hips talk to you again-when they whisper, ‘I’m ready.’ Not when your coach yells, ‘You’re cleared.’
Arthritis isn’t the endgame. It’s the consequence of ignoring the whispers until they become screams. And we treat athletes like machines that need tune-ups, not bodies that need understanding. Maybe the real surgery isn’t in the OR. Maybe it’s in how we think about movement. Maybe we need to stop fixing hips and start listening to them.
Jacqueline Aslet
November 28, 2025 AT 23:12While the clinical utility of magnetic resonance arthrography is indisputable, one cannot overlook the systemic inequities inherent in the dissemination of such diagnostic modalities. The socioeconomic stratification of orthopedic care, wherein access to MRA is contingent upon insurance coverage or personal wealth, constitutes a profound ethical dilemma in contemporary sports medicine. One must question whether the pursuit of optimal outcomes is being subordinated to fiscal pragmatism.
Caroline Marchetta
November 30, 2025 AT 20:53Oh wow, so we’re just supposed to believe that a $1,800 scan is the answer to everything? And no one’s talking about how most athletes are forced to ‘tough it out’ because their ‘team doctor’ is just a guy who graduated in 2015 and thinks ice baths fix everything? And then you get the ‘rehab’ that’s just yoga with a clipboard? I cried in PT last week because my therapist said ‘just stretch your hip flexors’ like I haven’t been doing it for 18 months. And now I’m supposed to be grateful because someone invented a ‘bioabsorbable anchor’? Like that’s gonna fix the fact that nobody taught me how to move correctly before I tore it?
And don’t even get me started on the ‘55% avoid surgery with PRP’ stat. That’s 55% of people who probably would’ve gotten better anyway. It’s placebo with a price tag.
katia dagenais
December 1, 2025 AT 17:09Let’s be real-most of these ‘success stories’ are from athletes who had access to elite clinics. The guy who got his hip fixed at a university hospital? He’s fine. The kid in rural Saskatchewan who got a regular MRI and was told ‘it’s just bursitis’? He’s now on disability at 31. This isn’t medicine. It’s a lottery. And the worst part? The system rewards the ones who can fight for care, not the ones who need it most. You think PRP is expensive? Try living with chronic hip pain while working two jobs and no benefits. No one talks about that. They just talk about anchors and 3D scans like we’re all living in a sci-fi movie.
And the ‘92% satisfaction’ at sports centers? That’s because they’re surrounded by people who can afford to take 6 months off. The rest of us are just hoping we don’t need surgery until after our rent is paid.
They say ‘your body is your tool.’ But what if your tool was broken by the very system that’s supposed to protect it? What then? Do we just buy a new one? There’s no upgrade path for a human.
Shirou Spade
December 2, 2025 AT 23:23There’s something poetic in how the hip-this joint that carries us through life, from first steps to final strides-gets treated like a replaceable part. We fix the tear, but never ask why the tear happened. We patch the cartilage, but never correct the imbalance that crushed it. The body doesn’t break randomly. It breaks in patterns. And those patterns? They’re written in our movement, our habits, our haste. Maybe the real surgery isn’t the one they do in the OR. Maybe it’s the one we do in our minds-learning to move with awareness, not just force. The hip doesn’t need fixing. It needs understanding.