What Is Hemochromatosis?
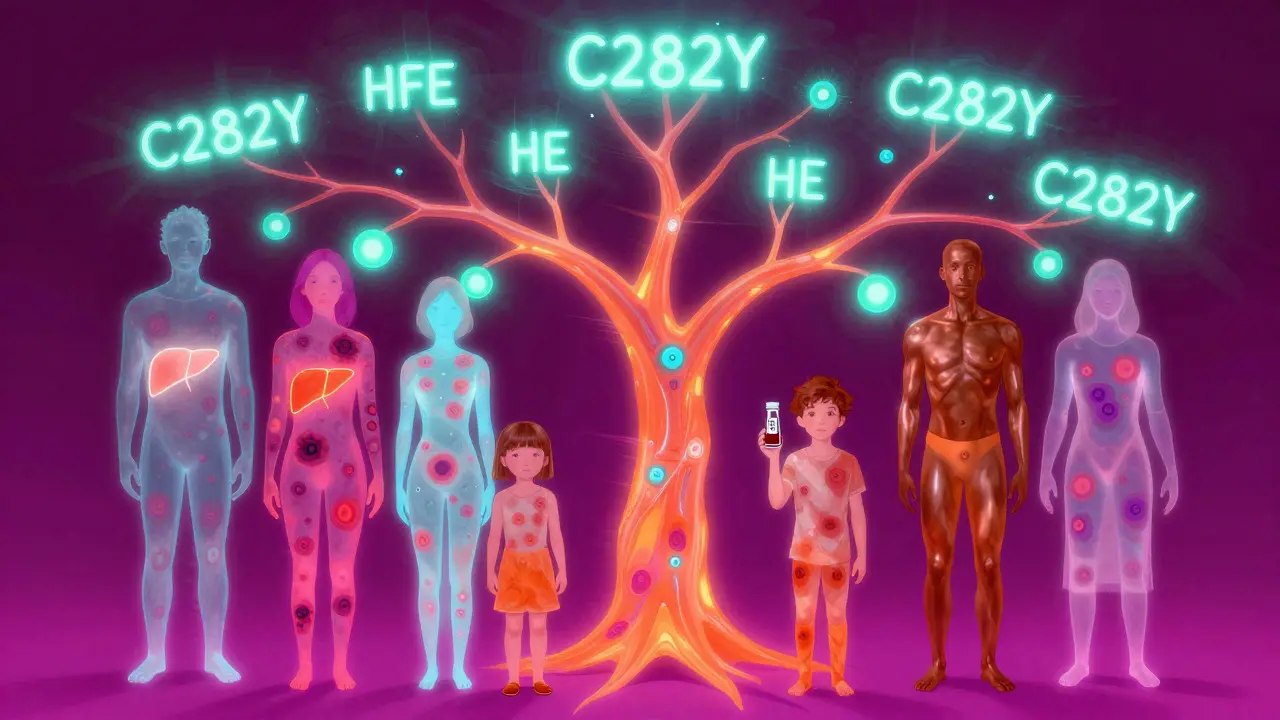
Hemochromatosis is a genetic disorder where the body absorbs too much iron from food, storing it in organs like the liver, heart, and pancreas until it causes damage. It’s not caused by eating too much iron-it’s your genes. Most cases come from a mutation in the HFE gene, especially the C282Y variant. If you inherit two copies-one from each parent-you’re at high risk. About 1 in 200 people of Northern European descent carry this double mutation. In Ireland, Scotland, and Wales, it’s even more common: 1 in 83 people have it.
Iron isn’t bad. Your body needs it to make red blood cells. But when you absorb 10 times more than you should, it builds up like rust inside your organs. Left untreated, that rust can scar your liver, mess with your heart rhythm, and even trigger diabetes. The good news? If caught early, it’s one of the easiest serious conditions to treat.
Why Do Symptoms Show Up So Late?
Most people with hemochromatosis feel fine for decades. Symptoms usually start between ages 30 and 50 in men. Women often don’t show signs until after menopause because monthly blood loss helps clear excess iron. That’s why men are diagnosed five to ten times more often.
Early symptoms are vague and easily mistaken for other things: constant tiredness, joint pain (especially in the knuckles), loss of sex drive, or erectile dysfunction. Many patients see three to five doctors over five to seven years before getting the right diagnosis. One Reddit user shared that after eight years of unexplained pain and fatigue, his ferritin level hit 2,850 ng/mL-more than ten times the normal range.
By the time skin turns bronze or gray, or you develop abdominal pain or diabetes, the damage is already underway. About 25% of patients develop type 2 diabetes because iron destroys insulin-producing cells in the pancreas. Around 45% develop skin discoloration. And if ferritin climbs above 1,000 ng/mL, there’s a 50-75% chance of cirrhosis.
How Is It Diagnosed?
Doctors don’t guess-they test. The first step is a simple blood panel: serum ferritin and transferrin saturation.
- Serum ferritin measures stored iron. Normal is under 300 ng/mL for men, under 200 ng/mL for women. Levels over 1,000 mean serious iron overload.
- Transferrin saturation shows how much iron is floating in your blood. Above 45% is a red flag. In secondary iron overload (like from blood transfusions), this number stays normal-so this test helps tell hemochromatosis apart from other causes.
Once those numbers are high, genetic testing confirms it. The HFE gene test looks for C282Y, H63D, and S65C mutations. C282Y homozygosity (two copies) explains 80-95% of cases. Other types exist, but they’re rare.
Today, liver biopsy is rarely needed. MRI scans with R2* technology can now measure liver iron precisely without needles. That’s a big win-no more 0.1% risk of bleeding or infection from a biopsy.

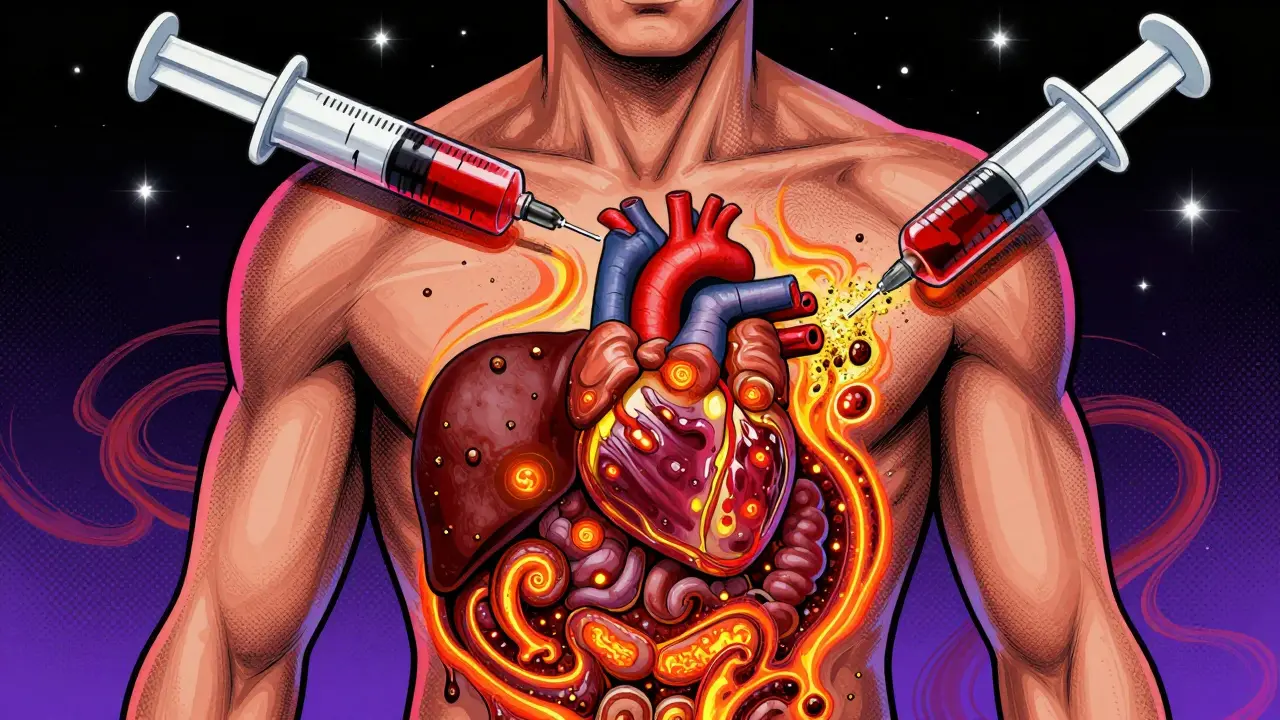
Phlebotomy: The Simple Treatment That Works
The treatment for hemochromatosis is straightforward: remove blood. Regularly. Just like donating blood-but it’s medical therapy, not charity.
Each phlebotomy removes about 500 mL of blood, which contains 200-250 mg of iron. Your body doesn’t make new red blood cells fast enough to replace the lost iron, so your stored iron drops.
There are two phases:
- Induction phase: Weekly sessions until ferritin hits 50-100 ng/mL. For someone with ferritin over 2,000, that could take 30-60 sessions over 12-18 months.
- Maintenance phase: Once iron is under control, you switch to every 2-4 months to keep ferritin in the safe zone. Most people need 4-6 sessions per year for life.
It’s cheap, too. Each session costs $0-$50, often covered by insurance. Compare that to iron-chelating drugs like deferasirox, which cost $25,000-$35,000 a year and come with side effects like nausea and kidney stress.
Patients report huge improvements: energy returns, joint pain fades, skin color normalizes. One survey found 89% satisfaction with phlebotomy once they got into maintenance. But here’s the catch: 42% quit after a few years because they feel fine. That’s dangerous. Stopping treatment lets iron creep back up. The damage doesn’t reverse-it just stops getting worse.
What Happens If You Don’t Treat It?
Untreated hemochromatosis is silent until it’s too late. Iron doesn’t just sit around-it attacks.
- Liver: Starts with fatty changes, then fibrosis, then cirrhosis. Once cirrhosis sets in, your risk of liver cancer jumps 20-fold.
- Heart: Iron deposits can cause arrhythmias or heart failure. This is rare but deadly.
- Pancreas: Leads to diabetes that’s hard to control.
- Endocrine system: Low testosterone, missed periods, infertility.
Survival rates tell the story: if you’re diagnosed before ferritin hits 1,000 ng/mL, your 10-year survival is 95%. If you’re diagnosed with cirrhosis, it drops to 60%. That’s not a gamble you want to take.
Who Should Get Tested?
Testing isn’t for everyone-but it should be for certain people:
- Anyone with unexplained high liver enzymes (ALT, AST)
- People with type 2 diabetes and no obesity or family history
- Those with joint pain in the knuckles, especially if it’s not rheumatoid arthritis
- Men over 30 with chronic fatigue or low libido
- First-degree relatives of someone diagnosed with hemochromatosis
Family screening is the most effective public health strategy. About 70% of cases are found after one person in the family is diagnosed. If your parent or sibling has it, get tested-even if you feel fine. The test is $150-$300 now, down from $1,200 in 2000.
The U.S. Preventive Services Task Force says there’s not enough evidence to screen the general population. But in Europe, doctors routinely test anyone with unexplained liver disease or heart problems. That’s smarter. Early detection saves lives-and money. Treating someone costs about $500 a year. Letting them develop cirrhosis? Over $42,000.
What’s Next for Treatment?
Phlebotomy works, but it’s not perfect. Some people have hard-to-access veins. Others get anemic or tired from frequent visits. Researchers are working on better options.
One promising drug, PTG-300, mimics hepcidin-the hormone your body stops making in hemochromatosis. In early trials, it lowered transferrin saturation by 53% in 12 weeks. If approved, it could mean injections instead of needles.
Scientists are also building polygenic risk scores. Instead of just looking at HFE, they’re combining 27 genetic markers to predict who will develop severe iron overload. Accuracy is now 89%. That could help identify at-risk people before symptoms even start.
For now, though, phlebotomy is still the gold standard. It’s proven, safe, and free of side effects when done right.
Living With Hemochromatosis
Once you’re on maintenance, life returns to normal. You can eat meat, drink alcohol in moderation, and live without restrictions. But there are a few things to avoid:
- Iron supplements: Even multivitamins with iron can undo progress.
- Vitamin C with meals: It boosts iron absorption. Take it separately.
- Raw shellfish: People with liver damage are at risk of serious infections from vibrio bacteria.
- Excess alcohol: It speeds up liver damage.
Regular blood tests every 3-6 months are non-negotiable. Your doctor should check ferritin and transferrin saturation-not just liver enzymes. And if you’re on maintenance, don’t skip your appointments. Feeling fine isn’t a reason to stop.
Support groups like the American Hemochromatosis Society and online forums help people stay on track. Many patients say knowing they’re not alone makes the lifelong treatment easier to stick with.
Can hemochromatosis be cured?
No, it can’t be cured-it’s a genetic condition. But it can be fully managed. With regular phlebotomy, iron levels stay in the safe range, organs stop getting damaged, and life expectancy returns to normal. You don’t need to live with symptoms or fear complications.
Is phlebotomy the same as donating blood?
It’s physically the same, but legally and logistically different. Therapeutic phlebotomy is prescribed by a doctor and done in a clinical setting. Blood donation centers usually won’t accept it unless they have a special program. Some patients use donation centers if their insurance covers it, but many go to hospitals or specialized clinics.
Can you get hemochromatosis from eating too much red meat?
No. You can’t get hereditary hemochromatosis from diet. It’s caused by genes. But eating large amounts of red meat or iron-fortified foods can make iron overload worse if you already have the gene mutation. The problem isn’t what you eat-it’s what your body does with it.
If my ferritin is high, does that mean I have hemochromatosis?
Not necessarily. High ferritin can come from alcohol use, obesity, inflammation, or liver disease. But if your transferrin saturation is also above 45%, and you have symptoms like fatigue or joint pain, hemochromatosis is likely. Genetic testing is the only way to know for sure.
How often do I need blood tests after starting treatment?
During the induction phase, every 4-6 weeks. Once you’re in maintenance, every 3-6 months. Your doctor will adjust based on your ferritin levels. Some people need testing every 2 months; others can stretch to 6 months if they’re stable.
Can women with hemochromatosis have children?
Yes, absolutely. Many women with hemochromatosis have healthy pregnancies. But iron overload can affect fertility and increase miscarriage risk if untreated. If you’re planning a pregnancy, get your ferritin under 100 ng/mL first. Treatment doesn’t stop during pregnancy-you may need to adjust phlebotomy frequency. Always work with a specialist.
What to Do Next
If you’ve had unexplained fatigue, joint pain, or high liver enzymes for months or years, ask your doctor for a ferritin and transferrin saturation test. It’s two simple blood draws. If you have a family member with hemochromatosis, get tested-even if you feel fine. Early detection is everything.
And if you’ve been diagnosed? Don’t wait. Start treatment. Stick with maintenance. Your liver, heart, and future self will thank you.
caroline hernandez
February 3, 2026 AT 16:53As a hematologist, I can't stress this enough: ferritin >1000 ng/mL is a red flag that demands immediate intervention. The liver fibrosis cascade begins silently, and by the time jaundice or ascites appears, you're already in decompensated cirrhosis territory. Phlebotomy isn't just therapy-it's organ preservation. I've seen patients with HFE homozygosity normalize their ALT/AST within 6 months of weekly sessions. The data is unequivocal: early phlebotomy reduces liver-related mortality by 82%. Don't wait for symptoms. Test. Treat. Survive.
Also, vitamin C with meals? Absolute no-go. Ascorbic acid increases non-heme iron absorption by up to 300%. Recommend taking it at bedtime instead. And for god's sake, avoid iron-fortified cereals if you're genetically predisposed. This isn't about diet-it's about gene expression.
Jhoantan Moreira
February 4, 2026 AT 06:31Just got my ferritin results back-2100. 😳 I thought I was just ‘burnt out’ from work. Turns out I’m a C282Y homozygote. Started phlebotomy last week. Feels weird to be ‘donating’ blood but getting paid in energy. My joint pain? Gone in 3 sessions. My wife says I’ve stopped groaning at 3 a.m. 🙌
Also-shoutout to the doc who ordered the test after I mentioned my dad had ‘liver issues’ in the 90s. Family screening saves lives. I’m getting my sister tested next week. 💙
Shelby Price
February 5, 2026 AT 18:34So… if I’m a woman with two copies of C282Y but never had symptoms before menopause, does that mean my body was just naturally doing phlebotomy for me? Wild. Feels like evolution gave us a built-in safety net. I’m 47, just diagnosed. My ferritin was 1800. I’m shocked I made it this far without knowing. Also, why isn’t this part of routine bloodwork? Like… ever? Seems like a no-brainer.
Sherman Lee
February 6, 2026 AT 05:54Let’s be real. The ‘genetic disorder’ narrative is convenient. Who benefits? Pharma? Blood centers? The CDC? They push phlebotomy because it’s cheap for them. But what about the iron chelation drugs? Why aren’t we researching oral alternatives? Why is the FDA still stuck in the 1980s? And why do they say ‘no cure’? It’s a mutation-not a death sentence. Maybe we should be editing genes, not draining blood. I’ve read papers on CRISPR trials in mice. But no one talks about it. Coincidence? I think not. 🤔
Lorena Druetta
February 6, 2026 AT 17:10To anyone reading this who feels overwhelmed: You are not alone. I was diagnosed at 34 after a routine work physical. I thought I was just tired. Now, I do maintenance phlebotomy every 8 weeks. I have energy. I sleep through the night. I play with my kids without needing a nap. It’s not glamorous. But it’s life-changing. I’ve been on this journey for 9 years. I’m alive. I’m here. And you can be too. One bag of blood at a time. You’ve got this. 💪
Nathan King
February 6, 2026 AT 21:14While the clinical efficacy of phlebotomy is well-documented, one must interrogate the epidemiological framing. The emphasis on Northern European ancestry risks biological essentialism. Iron overload phenotypes exist in sub-Saharan African and East Asian populations, often misclassified as ‘secondary’ due to diagnostic bias. The HFE-centric model is a Eurocentric artifact. Genetic testing panels must evolve beyond C282Y/H63D. We are neglecting global populations under the guise of ‘rare mutation’ dogma.
Harriot Rockey
February 7, 2026 AT 18:22Just had my first phlebotomy and I’m crying. Not from pain-because it was literally nothing-but because I finally understand why I’ve felt like a ghost for 12 years. My doctor said, ‘You’re not broken. You’re just overloaded.’ I’ve been taking iron supplements for ‘anemia’ since college. Turns out I was poisoning myself. 🤯
Thank you for this post. I’m telling my mom to get tested. And my coworkers. And my barista. This needs to be common knowledge. 💛
rahulkumar maurya
February 8, 2026 AT 21:17Phlebotomy? How quaint. In India, we treat iron overload with Ayurvedic herbs like Phyllanthus niruri and curcumin-based formulations. The Vedic texts describe ‘Lohaja Vikara’-iron imbalance-over 3000 years ago. Modern medicine is still stuck in the bloodletting era. Why not explore natural chelators? Why not integrate traditional knowledge? Western medicine is arrogant. It calls this ‘genetic’ and ignores holistic systems that have managed this for millennia.
pradnya paramita
February 10, 2026 AT 01:33As a lab specialist, I’ve seen 800+ ferritin samples over 7 years. The most common misdiagnosis? Non-alcoholic fatty liver disease (NAFLD). 40% of NAFLD patients with elevated ferritin turn out to be HFE homozygotes. Transferrin saturation >45% is the golden key. If you see high ferritin + normal CRP + no obesity, run the HFE panel. Don’t wait. Don’t assume. Test. Also-PTG-300 phase 2 data is promising. Hepcidin mimetics could revolutionize compliance. Imagine one injection every 4 weeks instead of 6 venipunctures. That’s the future.
Jamillah Rodriguez
February 12, 2026 AT 01:32Ugh. I just got diagnosed. Now I have to go to the hospital every 2 months? And I can’t have wine with dinner? And I have to tell my whole family? This is so annoying. I just wanted to be tired and eat steak. Why does this have to be a thing? 😭