Most people expect side effects from medications to show up right away - nausea after taking an antibiotic, dizziness after a blood pressure pill. But what if your body doesn’t react until days or even weeks later? That’s when you’re dealing with a delayed drug reaction, a type of immune response that catches many patients - and even some doctors - off guard.
Why Do Some Reactions Take So Long?
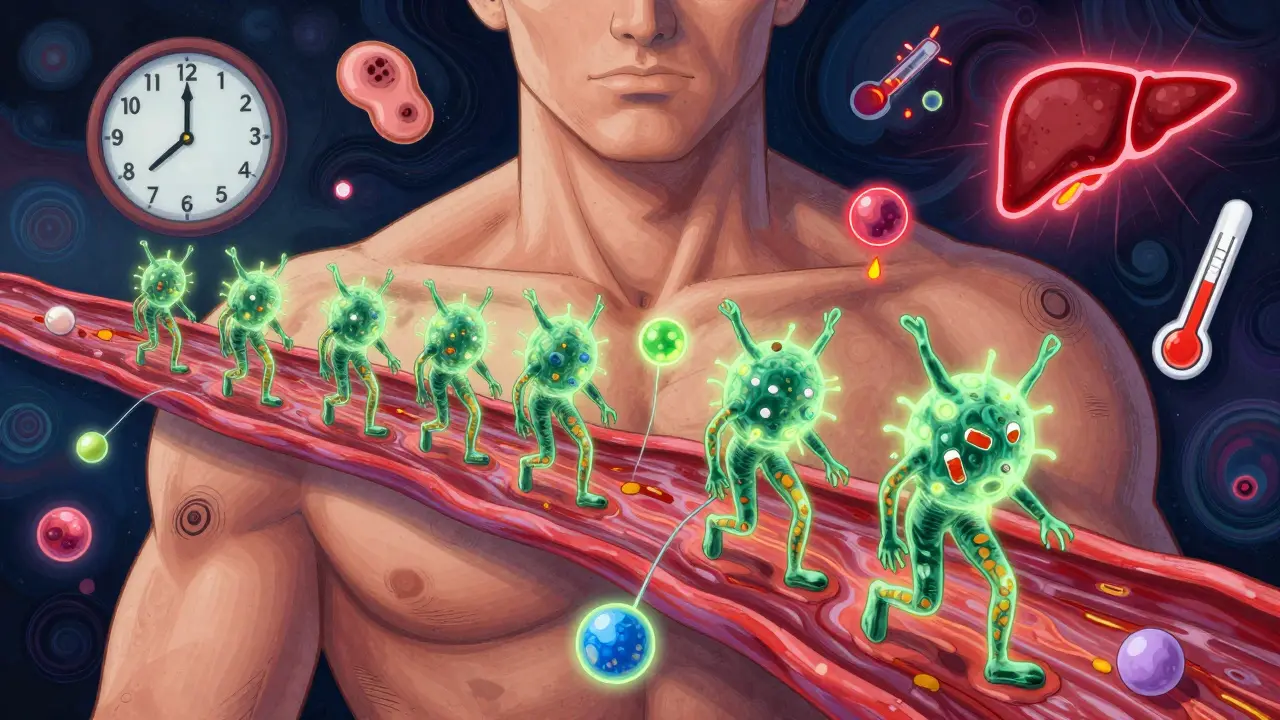
Unlike immediate allergic reactions (like hives or anaphylaxis that hit within minutes), delayed reactions are driven by your T-cells, not IgE antibodies. These immune cells don’t act fast. They need time to recognize the drug as a threat, multiply, and march to your skin, liver, or other organs. This process can take 5 to 8 weeks. That’s why a rash that shows up on day 12 after starting a new medicine isn’t just bad luck - it’s likely your immune system finally waking up.
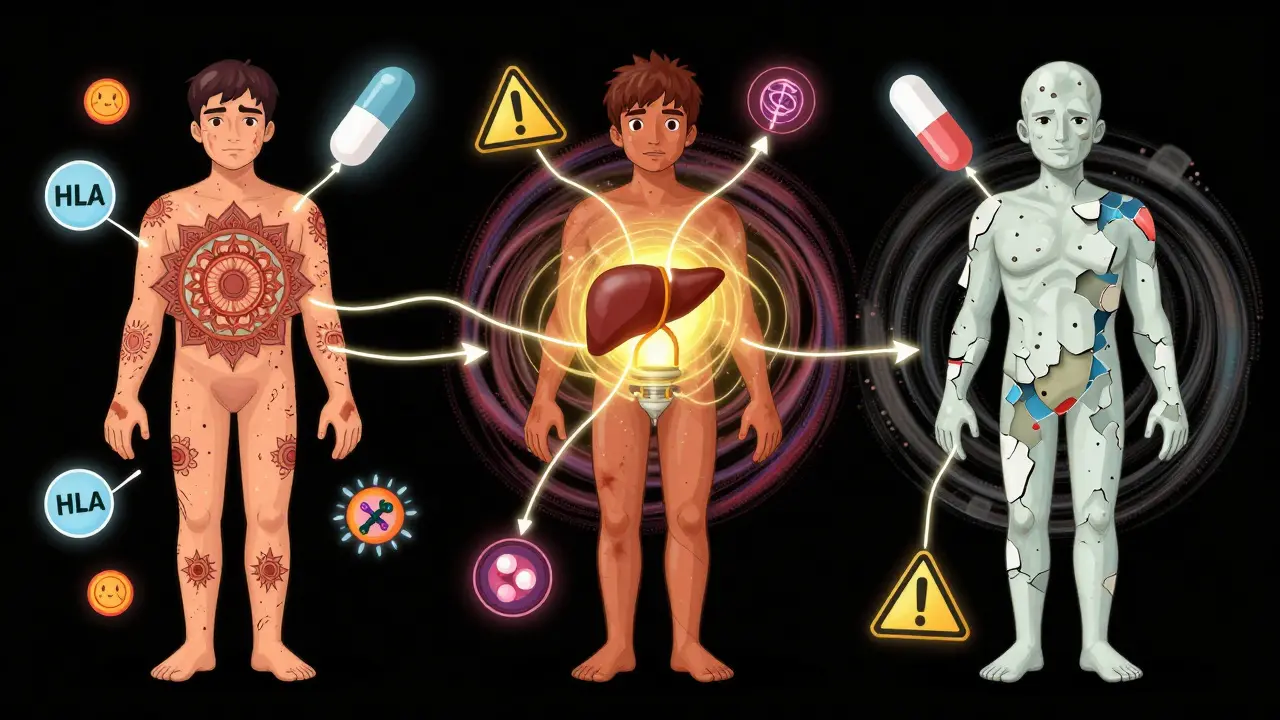
There are three main ways drugs trigger this:
- Hapten theory: The drug sticks to your body’s proteins, turning them into something your immune system sees as foreign.
- p-i concept: The drug directly binds to immune receptors, tricking T-cells into reacting - this explains up to 80% of cases.
- Altered peptide model: The drug changes how your cells present normal proteins, making them look like invaders.
Genetics play a huge role too. If you carry the HLA-B*15:02 gene, taking carbamazepine (a seizure drug) can trigger Stevens-Johnson Syndrome - a life-threatening skin reaction. In Southeast Asia, where this gene is common, doctors screen for it before prescribing. In Europe, where the gene is rare, this isn’t routine. That’s why the same drug can be safe for one person and deadly for another.
Common Delayed Reactions and When They Show Up
Not all delayed reactions look the same. Here are the most common types, with their timing and symptoms:
- Maculopapular exanthema (MPE): The most common. A flat, red rash with small bumps. Appears in 80-90% of cases, usually 8 days after starting the drug (range: 4-14 days). Often mistaken for a virus. It fades slowly - sometimes for weeks after you stop the medication.
- Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS): A full-body crisis. Fever above 38.5°C, swollen lymph nodes, high eosinophils (a type of white blood cell), and atypical lymphocytes. Onset: 2-8 weeks. Liver damage is common - some patients see ALT levels spike over 1,000 U/L. Recovery can take months. Relapses are possible even after symptoms seem gone.
- Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN): SJS affects less than 10% of skin surface; TEN more than 30%. Blisters, peeling skin, painful mucous membranes. Onset: 1-2 weeks. Mortality: up to 10% for SJS, over 30% for TEN with large skin loss.
- Acute Generalized Exanthematous Pustulosis (AGEP): Hundreds of tiny, sterile pustules covering the body. Comes on fast - within 2-3 days - but is usually gone within 15 days of stopping the drug. Often triggered by antibiotics like amoxicillin.
One patient, described in a 2023 Reddit thread, took lamotrigine for epilepsy. On day 22, they developed a 39.5°C fever, swollen glands, and liver enzymes 1,240 U/L. It took five months to fully recover. That’s DRESS - and it’s not rare.
Which Drugs Are Most Likely to Cause Delayed Reactions?
Some drugs are notorious for these delayed responses:
- Anticonvulsants: Carbamazepine, phenytoin, lamotrigine - often cause reactions after 2+ weeks. Carbamazepine is linked to HLA-B*15:02 in Asian populations.
- Antibiotics: Especially penicillins and sulfonamides (like sulfamethoxazole). Most reactions happen within 2 weeks.
- Allopurinol: Used for gout. Triggers DRESS and SJS/TEN. HLA-B*58:01 carriers are at extremely high risk - nearly 100% in some Thai populations.
- NSAIDs: Ibuprofen, naproxen. Can cause MPE or AGEP, often after prolonged use.
- ACE inhibitors: May cause delayed angioedema or rash after weeks of use.
According to FDA data from 2022, antibiotics cause 32% of delayed reaction reports, anticonvulsants 24%, and NSAIDs 18%. That’s why doctors often ask: “When did you start this drug?” - not just “What symptoms do you have?”
Why Diagnosis Is So Hard
Delayed reactions are sneaky. They look like:
- Viral rashes (measles, mononucleosis)
- Autoimmune diseases
- Secondary infections
One study found that 32% of early DRESS cases were misdiagnosed as infections. Patients get antibiotics - which makes things worse. In 28% of beta-lactam-induced reactions, doctors kept giving the drug, leading to 40% more complications.
There’s no single blood test. Diagnosis relies on:
- Timing: Did symptoms start 5-50 days after starting the drug?
- Clinical features: Does it match RegiSCAR criteria? (Fever, rash, organ involvement)
- Exclusion: Ruling out infections, other drugs, autoimmune causes
The Naranjo score (a tool doctors use) needs a score of 6 or higher to confirm a drug reaction. That’s not easy to hit without clear history.
What Happens After You Stop the Drug?
Stopping the drug is the most critical step - and it must happen within 48 hours of symptoms appearing. Delaying increases death risk by 35%, according to RegiSCAR data.
But stopping doesn’t mean healing. Symptoms often get worse before they get better. Why? The immune system is already activated. It takes time to shut down.
For MPE: Rash fades over 1-3 weeks. Skin may darken temporarily.
For DRESS: Improvement starts around 2 weeks, but relapse can happen at 3-4 weeks. Some patients need steroids for 4-8 weeks, tapered slowly. Cyclosporine is sometimes added for liver or kidney involvement - studies show it cuts recovery time by half.
For SJS/TEN: Skin regrows over 7-21 days. But scars, eye damage, and chronic pain can last years. 35% of survivors need lifelong eye care.
One patient on Inspire.com reported AGEP from sulfamethoxazole. The pustules vanished in 12 days - but the dark spots on their arms took six months to fade.
Testing and Prevention
Can we predict who’s at risk? Partially.
- HLA-B*58:01 screening before allopurinol is now recommended by the FDA for people of Asian descent. It can prevent 80% of severe reactions.
- HLA-B*15:02 screening for carbamazepine is standard in Thailand and Taiwan - and has cut SJS cases by over 90% in those populations.
- New blood tests are emerging: CXCL10 levels above 150 pg/mL predict DRESS severity with 87% accuracy.
- TCR sequencing (looking at T-cell receptors) is 92% sensitive for carbamazepine-SJS - but it’s still research-only.
But here’s the hard truth: current genetic tests explain only 40-60% of risk. Many people with no known genetic markers still react. We still can’t predict everyone.
For now, the best defense is awareness. If you’ve had a rash after a drug - even if it was mild - tell your doctor. Keep a list of medications that caused reactions. Future prescriptions should avoid those drugs entirely.

Long-Term Impact
Delayed reactions aren’t just acute events. They change lives.
- 68% of DRESS patients were hospitalized for over 10 days.
- 42% had severe liver damage.
- 28% had kidney injury.
- 22% developed autoimmune diseases within two years.
- 41% reported lasting anxiety about future medications.
One Reddit user wrote: “I can’t take any new antibiotic without panic. Every rash I get now - even from a virus - I think: ‘Is this it again?’”
And it’s not just emotional. A 2023 study found DRESS patients lost 23% of work productivity for six months after recovery. Medical costs? $112,500 per SCAR case. That’s more than a year’s rent in many places.
What to Do If You Suspect a Delayed Reaction
Don’t wait. Don’t assume it’s “just a virus.” Here’s what to do:
- Stop the drug immediately - even if you think it’s helping. This is the single most important step.
- Call your doctor - don’t wait for your next appointment. Describe the timing: “I started this on X date, and the rash started on Y date.”
- Take photos - rashes change fast. Photos help doctors track progression.
- Don’t take other new drugs - especially antibiotics or NSAIDs. They can make things worse.
- Keep a drug reaction log - write down every medication you take and any symptoms. This saves lives in the future.
If you’re hospitalized, ask: “Could this be DRESS or SJS?” Many ERs still don’t screen for it.
Final Thought
Delayed drug reactions are invisible until they’re not. They don’t show up on a lab report or an X-ray. They show up in your skin, your liver, your eyes - and sometimes, they show up too late.
But knowledge is power. If you’ve had a rash after a medication - no matter how mild - you’re not alone. And you’re not just “sensitive.” Your body gave you a signal. Listen to it. Tell your doctor. Keep track. Because next time, it might save your life.
Can a delayed drug reaction happen after I’ve stopped taking the medicine?
Yes. The immune system doesn’t shut off the moment you stop the drug. In DRESS syndrome, symptoms often peak 2-4 weeks after stopping the medication. Rashes can worsen, fever can return, and liver enzymes can spike. This is why doctors advise continuing monitoring for up to 6 weeks after discontinuation.
Are delayed drug reactions the same as allergies?
Not exactly. Immediate allergies (like anaphylaxis) are IgE-mediated and happen within minutes. Delayed reactions are T-cell mediated - they’re still immune responses, but they’re not classic “allergies.” Many doctors call them “drug hypersensitivity” to avoid confusion. The treatment is different too: antihistamines won’t help a DRESS reaction - steroids will.
Can I take the same drug again if I had a mild delayed reaction?
No. Even if your first reaction was mild - like a small rash - re-exposure can trigger a life-threatening reaction. Studies show a 75% chance of recurrence, and the second reaction is often worse. Once you’ve had a delayed hypersensitivity reaction to a drug, avoid it for life. Cross-reactivity is common - for example, if you reacted to carbamazepine, you’re likely to react to oxcarbazepine too.
Is there a blood test to confirm a delayed drug reaction?
There’s no routine blood test. Doctors rely on timing, symptoms, and exclusion of other causes. Specialized tests like lymphocyte transformation tests (LTT) exist but are only available in research labs or major allergy centers. They’re 75-85% sensitive but not widely used because they’re slow and expensive. Patch testing can help for some drugs (like topical antibiotics) but not for systemic reactions.
Can delayed drug reactions be prevented?
In some cases, yes. Genetic screening before prescribing can prevent most severe reactions. For example, testing for HLA-B*58:01 before giving allopurinol to people of Asian descent reduces DRESS and SJS risk by over 80%. But for most people, prevention comes down to awareness: knowing your history, telling your doctors, and avoiding drugs you’ve reacted to before. There’s no universal screening - yet.
Mike Hammer
February 15, 2026 AT 10:37Daniel Dover
February 15, 2026 AT 11:52Joe Grushkin
February 17, 2026 AT 03:19Mandeep Singh
February 17, 2026 AT 17:18Esha Pathak
February 18, 2026 AT 19:22Betty Kirby
February 19, 2026 AT 02:33Josiah Demara
February 19, 2026 AT 23:30Kaye Alcaraz
February 21, 2026 AT 16:30Erica Banatao Darilag
February 22, 2026 AT 21:29