Antibiotic Alternative Selector
Select Your Clinical Scenario
Quick Summary
- Cepmox is a brand of amoxicillin, a broad‑spectrum penicillin antibiotic.
- Common alternatives include penicillin V, azithromycin, doxycycline, clarithromycin, cephalexin and metronidazole.
- Choose an alternative based on infection type, bacterial resistance patterns, allergy history and dosing convenience.
- Amoxicillin remains first‑line for many ear, sinus and throat infections; alternatives are useful for resistant strains or penicillin‑allergic patients.
- Cost, side‑effects and treatment duration differ noticeably between options.
When a doctor prescribes an antibiotic, patients often wonder if there’s a better option. Cepmox vs alternatives is a common question, especially when side‑effects surface or when the infection doesn’t improve. This guide breaks down Cepmox (amoxicillin) and the most frequently used substitutes, helping you understand what each drug does, when it’s appropriate, and how it stacks up on price, safety and effectiveness.
What is Cepmox?
Cepmox is a branded formulation of amoxicillin, a beta‑lactam antibiotic belonging to the penicillin family. It was launched in the UK in 2018 and is marketed by a subsidiary of a multinational pharma group. Cepmox tablets typically contain 250mg or 500mg of amoxicillin per dose, designed for oral administration.
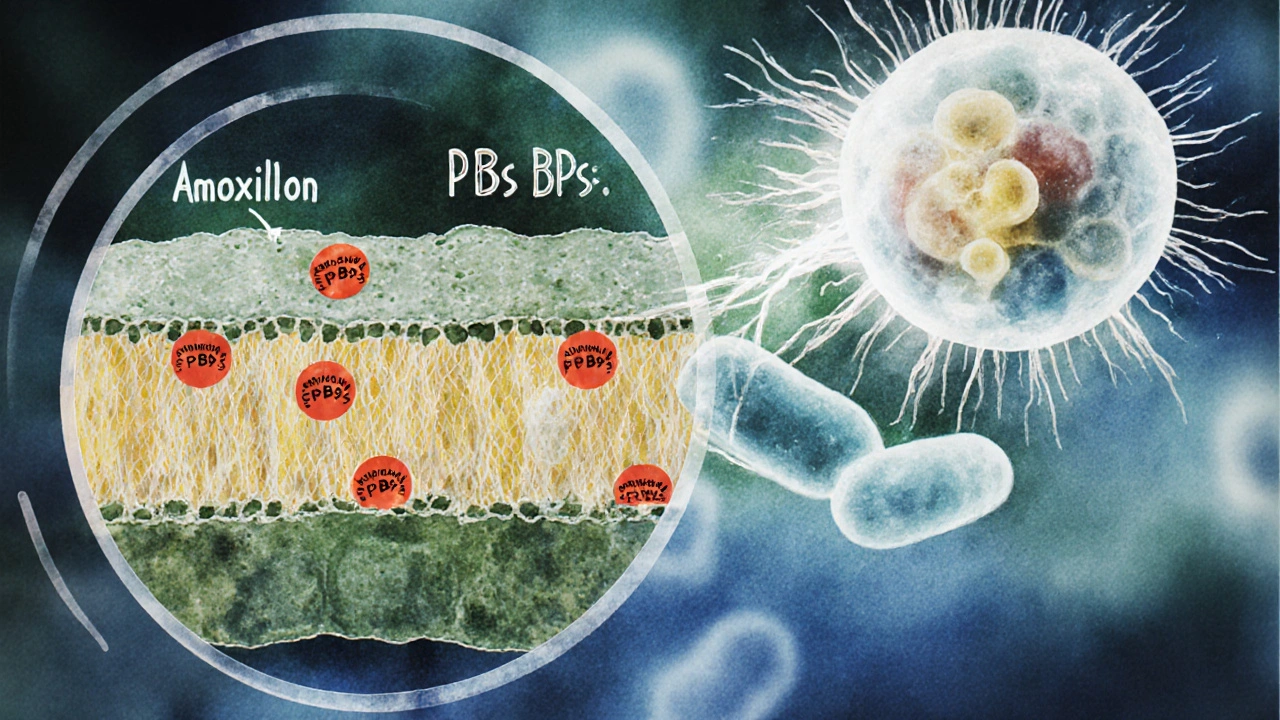
Amoxicillin works by inhibiting the synthesis of bacterial cell walls, leading to cell lysis and death of susceptible organisms. Its broad spectrum covers many gram‑positive and some gram‑negative bacteria, making it a go‑to for ear, sinus, throat and urinary‑tract infections.
How Amoxicillin (Cepmox) Works
Because amoxicillin is a penicillin derivative, it binds to penicillin‑binding proteins (PBPs) that are essential for peptidoglycan cross‑linking in bacterial cell walls. Disruption of this process weakens the wall, causing osmotic pressure to burst the cell.
Key attributes of amoxicillin:
- Absorption: ~90% oral bioavailability.
- Half‑life: Approximately 1 hour in healthy adults.
- Excretion: Primarily renal, so dose adjustment is needed for kidney impairment.
- Typical dosage: 500mg three times daily for 7‑10days in most adult infections.
The drug is generally well‑tolerated, but common side‑effects include mild gastrointestinal upset, rash and, rarely, allergic reactions that can be severe.
Common Alternatives to Cepmox
When amoxicillin isn’t suitable-due to allergy, resistance or specific infection type-clinicians switch to other agents. Below are the most common alternatives, each with its own spectrum and usage profile.
Penicillin V
Penicillin V (phenoxymethylpenicillin) is a narrow‑spectrum oral penicillin. It’s often chosen for streptococcal throat infections when the bacterial load is low and the patient can tolerate a short‑acting agent.
Azithromycin
Azithromycin belongs to the macrolide class. It has a long half‑life, allowing once‑daily dosing for 3‑5days, and is useful for atypical pathogens like Mycoplasma and Chlamydia.
Doxycycline
Doxycycline is a tetracycline antibiotic with activity against a wide range of bacteria, including some resistant strains. It’s frequently prescribed for acne, tick‑borne illnesses and certain respiratory infections.
Clarithromycin
Clarithromycin is another macrolide, offering better coverage of Haemophilus influenzae and atypical bacteria than azithromycin, though it requires twice‑daily dosing.
Cephalexin
Cephalexin is a first‑generation cephalosporin. It shares a beta‑lactam structure but is typically tolerated by patients with mild penicillin allergy, covering skin and soft‑tissue infections well.
Metronidazole
Metronidazole targets anaerobic bacteria and certain protozoa. It’s not a direct substitute for amoxicillin but is combined with it for mixed infections, such as dental abscesses.
Side‑Effect Profiles at a Glance
Understanding tolerability helps you decide which drug fits your lifestyle. Below is a concise side‑effect comparison.
| Antibiotic | Gastro‑intestinal upset | Allergic reaction risk | Typical dosing schedule | Special notes |
|---|---|---|---|---|
| Cepmox (Amoxicillin) | Mild nausea, diarrhea (≈10%) | 5-10% (potentially severe) | 3× daily | Renal dose‑adjustment needed |
| Penicillin V | Similar to amoxicillin | 5-10% | 4× daily | Shorter half‑life |
| Azithromycin | Less frequent, possible abdominal pain | ~2% (lower) | 1× daily (3‑5days) | Long tissue half‑life |
| Doxycycline | Esophageal irritation, photosensitivity | ~1% rash | 1-2× daily | Avoid with iron supplements |
| Clarithromycin | Diarrhea, taste disturbance | ~3% rash | 2× daily | Potential drug‑drug interactions (CYP3A4) |
| Cephalexin | Low‑grade nausea, abdominal cramp | ~2% (often milder than penicillin) | 2-3× daily | Often safe for mild penicillin allergy |
| Metronidazole | Metallic taste, nausea | ~1% rash | 2-3× daily | Avoid alcohol during and 48h after |
Decision Criteria: Picking the Right Antibiotic
Choosing an alternative isn’t a random guess. Use the following checklist to match the drug to your clinical scenario.
- Infection type: Respiratory (streptococcal), skin, urinary, dental, or atypical pathogens each have preferred agents.
- Pathogen susceptibility: Check local NHS antibiotic‑resistance data. For example, in 2024 England, Penicillin‑resistant Streptococcus pneumoniae rose to 12% in community cases.
- Allergy history: Any documented penicillin allergy steers clinicians toward macrolides or cephalosporins with low cross‑reactivity.
- Patient age and kidney function: Dosing adjustments for elderly or renal‑impaired patients often favor drugs with longer half‑lives (e.g., azithromycin).
- Convenience: Once‑daily regimens improve adherence, especially for working adults.
- Cost and NHS coverage: Generic amoxicillin remains the cheapest (<£2 for a 7‑day course), while azithromycin and clarithromycin are pricier but sometimes fully reimbursed for specific indications.
By ticking these boxes, you can rationalize why a doctor might prescribe Cepmox or switch you to an alternative.
Practical Tips & Safety Considerations
Regardless of the antibiotic you end up with, keep these habits in mind.
- Finish the entire prescribed course, even if symptoms improve early.
- Take the medication with a full glass of water; for doxycycline, stay upright for at least 30minutes to avoid oesophageal irritation.
- Report any rash, swelling or breathing difficulty immediately-these could signal an anaphylactic reaction.
- Avoid alcohol with metronidazole to prevent a disulfiram‑like reaction.
- Inform your pharmacist about any other meds, especially warfarin, statins or oral contraceptives, as macrolides can alter their effectiveness.
- Check the NHS website for the latest regional resistance patterns before requesting a specific antibiotic.
Frequently Asked Questions
Can I switch from Cepmox to another antibiotic if I get a rash?
Yes. A rash often signals a mild allergy. Your clinician can change you to a macrolide such as azithromycin or a cephalosporin like cephalexin, which many patients with mild penicillin allergy tolerate well.
Is amoxicillin still effective against most ear infections?
For uncomplicated acute otitis media caused by Streptococcus pneumoniae or Haemophilus influenzae, amoxicillin remains first‑line in the UK NHS guidelines, unless local resistance rates exceed 20%.
Why might a doctor prescribe azithromycin instead of Cepmox?
Azithromycin’s long half‑life allows a short, once‑daily regimen, which is handy for patients who struggle with three‑times‑daily dosing. It’s also chosen when the suspected pathogen is atypical (e.g., Mycoplasma) or when there’s known penicillin allergy.
Is it safe to take antibiotic leftovers from a previous prescription?
No. Using leftover antibiotics can promote resistance and may not treat the current infection effectively. Always get a fresh prescription based on a proper diagnosis.
How does antibiotic resistance affect the choice between Cepmox and alternatives?
If local data show high resistance to amoxicillin for a specific bug, clinicians will skip Cepmox and choose a drug with a different mechanism, such as doxycycline or a macrolide, to ensure efficacy.
By weighing infection specifics, allergy history, resistance trends and practical factors, you can understand why Cepmox (amoxicillin) may be the best fit-or why one of its alternatives is a smarter choice. Always discuss any concerns with your GP or pharmacist, and follow the prescribed course exactly for the safest outcome.

Avinash Sinha
October 11, 2025 AT 21:35Oh, the saga of Cepmox versus its kin reads like an epic novel! From the moment you pop that 500 mg tablet, you’re launching a micro‑battle against stubborn bacteria. The spectrum of amoxicillin sweeps across the respiratory corridors like a knight’s blade, yet the side‑effects whisper like mischievous sprites. If you’re allergic, the plot twist introduces azithromycin, the suave rogue with once‑daily charm. And let’s not forget the cost‑saving subplot that keeps the purse strings from weeping. In short, pick your hero wisely, lest the infection write its own tragic ending.
ADAMA ZAMPOU
October 12, 2025 AT 19:48In the clinical deliberation of antimicrobial selection, one must first ascertain the pathogen’s susceptibility profile. The comparative pharmacodynamics of amoxicillin and its alternatives reveal distinct advantages contingent upon infection locus. Moreover, consideration of renal function and potential hypersensitivity remains paramount to therapeutic success.
Liam McDonald
October 13, 2025 AT 18:01i get it antibiotics can be confusing but amoxicillin is often first line for ear infections it works well for many common bugs however if you have a penicillin allergy azithromycin is a good swap it’s taken once daily which helps with compliance also watch out for stomach upset with any of them
Adam Khan
October 14, 2025 AT 16:15The pharmacokinetic profile of amoxicillin is suboptimal compared to azithromycin.
rishabh ostwal
October 15, 2025 AT 14:28Let us not be blinded by the seductive allure of newer, pricier antibiotics when the venerable Cepmox stands ready to defeat the majority of community‑acquired pathogens. Its broad spectrum, coupled with a well‑established safety record, makes it the logical first choice for most clinicians. Yet the misguided obsession with “flashier” drugs often leads to unnecessary side‑effects and inflated healthcare costs. One must weigh the evidence, not the marketing hype, before abandoning a proven workhorse. In the grand theatre of medicine, prudence should outrank novelty.
Kristen Woods
October 16, 2025 AT 12:41Deaer readers, let me clinch the point-Cepmox is a stalwart, but if you’ve ever felt a rumbl on your tummy after a dose, you’re not alone. The alternatives, such as azithromyin, promise fewer GI issues, yet they come with their own quirks like potential heart rhythm changes. Costwise, generic amoxicillin often wins, but some pharmacies puchase the brand at a premium. In terms of dosing, once‑daily azithro is a dream for the busy, while amoxicillin demands threes a day. Ultimately, the choice hinges on allergy history, infection type, and your tolerance for a lil bit of inconvenience.
Carlos A Colón
October 17, 2025 AT 10:55Ah, the classic dilemma: “Do I stay loyal to my trusty amoxicillin or flirt with that fancy azithromycin?” It’s like choosing between a reliable old sedan and a sleek sports car that guzzles gas. If your gut is already staging a revolt, maybe swap the pill. Just remember, every antibiotic has its mood swings-some love the spotlight, others hide in the shadows of side‑effects. So pick the one that won’t make you feel like you’ve swallowed a cactus.
Aurora Morealis
October 18, 2025 AT 09:08Amoxicillin remains affordable and effective for most respiratory infections. Alternatives can be useful when allergies or resistance are concerns. Choose based on clinical guidelines.
Sara Blanchard
October 19, 2025 AT 07:21When we discuss antibiotics, it’s vital to honor the diverse experiences patients bring to the conversation. Some communities may have heightened concerns about side‑effects due to past medical mistrust. Providing clear, respectful information about Cepmox and its alternatives helps build confidence across cultures. Let’s ensure every voice feels heard and every choice is informed.
Anthony Palmowski
October 20, 2025 AT 05:35Look, folks-amoxicillin is the workhorse, the every‑day hero, and it gets the job done, but if you’ve got a penicillin allergy, you’re forced into the azithro lane, which, let’s be honest, is pricey, and sometimes it can cause QT prolongation, a real heart‑rhythm nightmare, plus the GI side‑effects aren’t exactly a picnic, so weigh the pros, cons, and your wallet before you pop that pill!
Jillian Rooney
October 21, 2025 AT 03:48It is often overlooked that amoxcillin, despite its widespread use, may not be the best fit for every patient, especially those with hidden renal issues. One should consider alternatives like doxycycline, which side‑steps many of the allergic reactions, yet many prescribrs ignore this nuance. The healthcare system sometimes pushes cheap options without full transparency. A more nuanced approach is required, though it is rarely adopted.
Rex Peterson
October 22, 2025 AT 02:01One might contend that the ethical stewardship of antibiotics demands a judicious balance between efficacy and the mitigation of resistance. In this regard, the selection of Cepmox versus a macrolide alternative embodies a microcosm of broader pharmacologic decision‑making. The practitioner must reconcile the immediate therapeutic imperative with the long‑term societal burden of antimicrobial tolerance.
Candace Jones
October 23, 2025 AT 00:15Choosing the right antibiotic begins with a clear diagnosis of the infection type, whether it be respiratory, skin, urinary, dental, or atypical. Once the diagnosis is established, the next step is to assess the patient’s allergy history, especially any documented penicillin hypersensitivity. If the patient tolerates penicillins, amoxicillin (Cepmox) remains the first‑line option for most common pathogens due to its proven efficacy and low cost. For patients with a true IgE‑mediated penicillin allergy, azithromycin offers a convenient once‑daily regimen with a favorable side‑effect profile. In cases of mild penicillin allergy where cross‑reactivity risk is low, cephalexin can be considered, particularly for skin and soft‑tissue infections. When dealing with atypical organisms such as Mycoplasma or Chlamydia, a macrolide like azithromycin or clarithromycin is preferred over amoxicillin. Renal function must be evaluated, as amoxicillin requires dose adjustment in moderate to severe impairment, whereas azithromycin does not. Age is another factor; elderly patients may benefit from the simpler dosing and reduced gastrointestinal upset of macrolides. Cost considerations are also important; generic amoxicillin is typically the most affordable, but insurance formularies may favor alternative agents in certain regions. The duration of therapy varies: amoxicillin often requires a 7‑10‑day course, while azithromycin can be completed in 3‑5 days, improving adherence. Side‑effects differ, with amoxicillin more likely to cause mild diarrhea and rash, while azithromycin may cause transient abdominal discomfort. Drug‑drug interactions should be reviewed, especially with clarithromycin, which inhibits CYP3A4. In pregnancy, amoxicillin is generally safe, whereas doxycycline is contraindicated. Finally, patient preference regarding dosing frequency and potential side‑effects should be incorporated into the shared decision‑making process. By systematically evaluating these variables, clinicians can tailor antibiotic therapy to achieve optimal outcomes while minimizing adverse events.
Robert Ortega
October 23, 2025 AT 22:28Thank you for outlining such a thorough framework; I will definitely apply these steps in my next patient encounter.