Carbamazepine Therapeutic Drug Monitoring Calculator
Carbamazepine therapeutic plasma levels should be maintained between 4-12 µg/mL for optimal seizure control. Levels above 15 µg/mL increase the risk of toxicity.
Enter your carbamazepine blood level to see if it falls within the therapeutic range.
Carbamazepine is a broad‑spectrum antiepileptic drug (AED) that has been used for more than six decades to control seizures and stabilize mood. Its popularity stems from a well‑documented track record, but many patients wonder why carbamazepine works so well. The answer lies in a mix of chemistry, neurophysiology, and the way the body handles the molecule.
How Carbamazepine Works: The Core Mechanism
At the cellular level, Sodium channel blocker describes the primary action of carbamazepine. Neurons fire by allowing sodium ions to rush in through voltage‑gated Na⁺ channels. Carbamazepine preferentially binds to the inactive state of these channels, prolonging their closed configuration. The result is a dampened neuronal firing rate, especially in hyper‑excitable regions of the brain that generate seizures.
Beyond sodium channels, carbamazepine has secondary effects on GABAergic transmission and glutamate release, subtly enhancing inhibitory signaling while suppressing excitatory bursts. This multimodal profile explains why the drug helps not only with focal seizures but also with generalized tonic‑clonic events.
Pharmacokinetics: How the Body Processes Carbamazepine
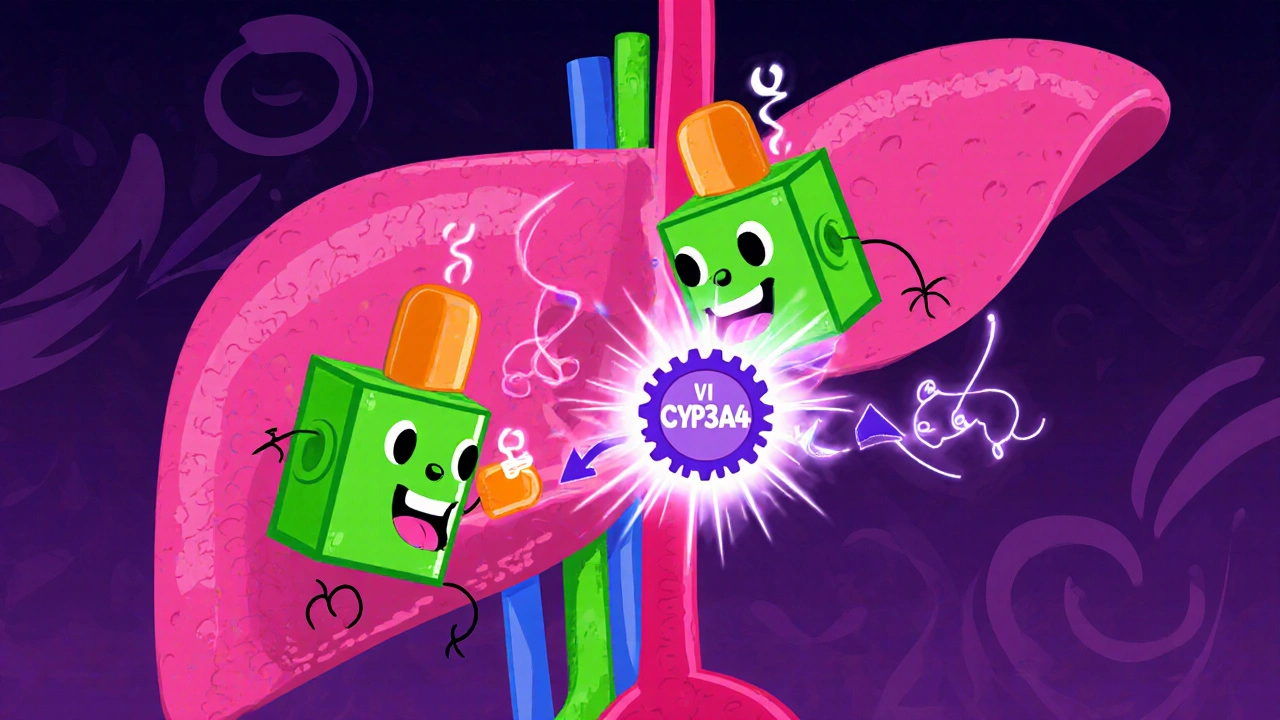
The journey from pill to brain follows a classic Pharmacokinetics curve. After oral administration, carbamazepine is rapidly absorbed (peak plasma levels in 4-6 hours) and undergoes extensive first‑pass metabolism in the liver. The key player in this metabolic pathway is the CYP450 enzyme CYP3A4, which converts the parent drug into its active metabolite carbamazepine‑10,11‑epoxide.
The epoxide is actually more potent at blocking sodium channels than the parent, contributing to therapeutic effect but also to toxicity if it accumulates. Because carbamazepine induces its own metabolism (auto‑induction), steady‑state concentrations typically require 2-3 weeks of consistent dosing.
Clinical Uses: From Seizure Disorders to Mood Stabilization
Originally approved for Seizure disorders, carbamazepine quickly found a niche in psychiatry. Its efficacy in treating the manic phase of Bipolar disorder is comparable to that of lithium, making it a valuable alternative for patients who cannot tolerate lithium’s side‑effects.
In epilepsy, carbamazepine shines for focal onset seizures, especially those arising from the temporal lobe. Clinical trials conducted in the 1990s showed a 60 % responder rate (≥50 % seizure reduction) in patients who were previously refractory to monotherapy.
Safety Profile, Adverse Effects, and Monitoring
Like any drug that alters neuronal excitability, carbamazepine carries a risk of Adverse effects. Common complaints include dizziness, drowsiness, and mild nausea. More serious concerns involve hematologic reactions such as aplastic anemia and agranulocytosis, which occur in roughly 1 per 10,000 patients.
Because the active metabolite can build up, clinicians rely on Therapeutic drug monitoring. Target plasma levels range from 4-12 µg/mL for seizure control; levels above 15 µg/mL increase the likelihood of toxicity. Routine blood counts are also recommended during the first six months of therapy.
Drug Interactions: The CYP450 Web
Carbamazepine’s status as a strong inducer of CYP450 enzyme CYP3A4 means it can lower the plasma concentrations of many co‑administered drugs-oral contraceptives, warfarin, and certain antiretrovirals are classic examples. Conversely, inhibitors of CYP3A4 (e.g., erythromycin, ketoconazole) can raise carbamazepine levels, heightening the risk of adverse effects.
When prescribing carbamazepine alongside other AEDs, the most frequent interaction is with Valproic acid. Valproate can inhibit epoxide hydrolase, causing epoxide accumulation and increasing neurotoxicity. Clinicians typically avoid this combination unless the therapeutic benefit clearly outweighs the risk.

How Carbamazepine Stacks Up Against Other AEDs
| Property | Carbamazepine | Valproic acid | Lamotrigine |
|---|---|---|---|
| Primary mechanism | Sodium channel blocker | Multiple: GABA ↑, Na⁺ channel block | Sodium channel blocker (weak) |
| Induction of CYP enzymes | Strong (CYP3A4) | Weak (CYP2C9) | Minimal |
| Effective seizure types | Focal, partial‑onset | Generalized, absence | Focal, generalized |
| Common adverse effects | Dizziness, rash, blood dyscrasias | Weight gain, tremor, hepatotoxicity | Skin rash (rare SJS) |
| Therapeutic plasma range (µg/mL) | 4‑12 | 50‑100 | 2‑14 |
The table makes it clear why carbamazepine remains a first‑line choice for focal epilepsy: its sodium‑channel specificity and long‑standing safety data outweigh the induction‑related drug‑interaction concerns for many patients.
Practical Tips for Patients and Providers
- Start low, go slow: typical initial dose is 100 mg twice daily, titrating by 200 mg every week.
- Schedule regular blood work: CBC every month for the first six months, then quarterly.
- Check contraceptive effectiveness: women on hormonal birth control should use backup methods or switch to non‑hormonal options.
- Review all current meds for CYP3A4 interactions-antibiotics, antifungals, and some antidepressants can change carbamazepine levels.
- Educate patients about rash warning signs; a sudden skin eruption may signal Stevens‑Johnson syndrome, which requires immediate discontinuation.
Frequently Asked Questions
How long does it take for carbamazepine to start working?
Therapeutic effects usually appear within 1-2 weeks, but full steady‑state concentrations may require 3-4 weeks due to auto‑induction.
Can carbamazepine be used during pregnancy?
It is classified as Category D; it crosses the placenta and is linked to a small increase in birth defects, so risk‑benefit analysis is essential.
What should I do if I develop a rash?
Stop the medication immediately and seek medical attention. Early discontinuation can prevent progression to severe skin reactions.
Does carbamazepine interact with alcohol?
Alcohol can amplify drowsiness and dizziness. It’s best to limit intake, especially during dose titration.
How is carbamazepine monitored in blood?
Therapeutic drug monitoring targets 4-12 µg/mL. Levels are checked 2-3 weeks after any dose change or when side effects appear.

Xavier Lusky
October 21, 2025 AT 16:32Ever since the 1960s the pharmaceutical giants have been pushing carbamazepine as the miracle seizure drug. What most people don’t realize is that the same companies finance the research that touts its “sodium channel blockade” as a breakthrough. The drug’s ability to bind the inactive state of Na+ channels is real, but it also conveniently masks the fact that it was designed to silence any neural activity that could reveal their hidden neuro‑surveillance programs. Those metabolites like carbamazepine‑10,11‑epoxide are not just therapeutic; they are engineered to keep the brain under a subtle chemical leash. Auto‑induction is presented as a pharmacokinetic curiosity, yet it is precisely the mechanism that forces patients to stay on the medication forever while the company profits from repeat prescriptions. The table comparing AEDs looks clean on paper, but the fine print shows a web of CYP3A4 interactions that can be exploited to control other drugs the patient might take. You’ll notice the article never mentions the corporate lobbying that got carbamazepine labeled “first‑line” despite safer alternatives existing. The “steady‑state” period of 2‑3 weeks is a perfect window for sales reps to schedule follow‑up appointments and lock patients into long‑term contracts. Even the warning about rash is understated; severe skin reactions have been weaponized in clinical trials to scare away competition. The mention of blood dyscrasias is a clue that the manufacturer knows how to weaponize side effects as a market differentiator. The fact that carbamazepine induces its own metabolism is not a coincidence; it is a built‑in feedback loop that keeps the drug’s plasma levels volatile, ensuring patients keep coming back for dose adjustments. The article’s “practical tips” sound like a checklist for a controlled substance distribution scheme. When you read about the drug’s effect on mood stabilization, ask yourself why the same molecule is also being investigated for off‑label uses in anxiety and aggression control in prisons. The “CYP450 web” is more like a spider that the pharma industry spins to catch any competing medication. In short, the science is real, but the narrative is curated to keep us dependent on a single, profit‑driven molecule. Stay skeptical and demand independent studies before you trust another “gold‑standard” drug.
Devendra Tripathi
October 28, 2025 AT 19:32You’re missing the bigger picture here. The article glosses over the fact that carbamazepine’s efficacy is highly patient‑specific and that many newer agents have a better safety profile. It’s not a one‑size‑fits‑all miracle drug, contrary to the hype. If you look at the recent meta‑analyses, the margin of benefit shrinks dramatically when you control for comorbidities.
Vivian Annastasia
November 4, 2025 AT 23:32Oh great, another “expert” breakdown that pretends to be helpful while ignoring the real-life nightmare of skin reactions. Sure, the sodium channel story is neat, but does it really matter when you’re staring at a rash that looks like it belongs on a horror movie? And the whole auto‑induction thing? Just another excuse for patients to feel guilty when they’re non‑compliant.
eric smith
November 12, 2025 AT 03:32Let’s get the basics straight: carbamazepine blocks the inactivated Na+ channels, nothing mystical about it. If you’re confused about the epoxide metabolite, it’s simply a more potent blocker, not a conspiratorial super‑drug. The drug’s history is well‑documented, no need for elaborate theories.
Jake Hayes
November 19, 2025 AT 07:32Carbamazepine’s primary indication remains focal seizures; its efficacy is well‑established. Avoiding polypharmacy when possible reduces interaction risk.
parbat parbatzapada
November 26, 2025 AT 11:32yo man the whole drug thing is like a drama series i cant even
the auto‑induction is like a sneaky plot twist that keeps us on edge
and dont even get me started on the rash saga its like a horror flick
Casey Cloud
December 3, 2025 AT 15:32Carbamazepine is absorbed quickly after oral intake and reaches peak plasma levels in about 4 to 6 hours without any major issues. Monitoring blood levels is essential especially after dose changes to keep you in the therapeutic window.
Rachel Valderrama
December 10, 2025 AT 19:32Wow, thanks for the “helpful” reminder about blood work – didn’t know doctors actually want us to get tested. Keep those tips coming, maybe next you’ll tell us to breathe.
John Price
December 17, 2025 AT 23:32Sounds like a solid plan.
Nick M
December 25, 2025 AT 03:32Honestly, carbamazepine is just another bullet in the pharma arsenal – it does its job, but the side‑effect profile is a jargon‑filled mess. You get the typical dizziness, nausea, and that dreaded blood dyscrasia risk that’s always mentioned in the fine print. The drug induces its own metabolism, so you’re stuck in a loop of dose adjustments that feels like a lazy dance. It’s effective for focal seizures, but if you’re looking for innovation, look elsewhere.
Erika Thonn
January 1, 2026 AT 07:32i think the carbamazepine is like a philosophikal mirror reflecting our minde but also like a trap dont you agree? the epoxied metabolite is the part tht shows how we cant trust anything . its like a paradox where we are both safe and at risk. maybe the drug is a metaphor for life itself, full of hidden complexities no one want to see. whatever it is, the science must keep evolving
Ashok Kumar
January 8, 2026 AT 11:32I get why patients feel nervous about side effects, especially the rash. At the same time, the drug’s efficacy can’t be denied for many who have refractory seizures. It’s a balance of risk and benefit, and the monitoring guidelines help mitigate serious issues. Still, the tone of the article could have been more empathetic.
Jasmina Redzepovic
January 15, 2026 AT 15:32Let’s be clear: carbamazepine is a cornerstone of American epilepsy treatment and any suggestion it’s a product of foreign conspiracies is pure nonsense. Our regulatory agencies have vetted its safety profile, and the data supports its continued use. Dismissing it as a “pharma tool” undermines the progress of our medical community. If you’re worried about interactions, just read the label and follow the guidelines. Anything else is just fear‑mongering.