High blood pressure doesn’t come with warning signs. You might feel fine, but your arteries are under constant strain. Left unchecked, it can lead to heart attack, stroke, or kidney failure. That’s why millions of people take blood pressure medications every day - not because they’re sick, but because they need to stay that way. The right drug can cut your risk of stroke by up to 40%. But choosing one isn’t just about lowering a number. It’s about matching your body, your other health issues, and even your lifestyle to the right treatment.
How Blood Pressure Medications Work
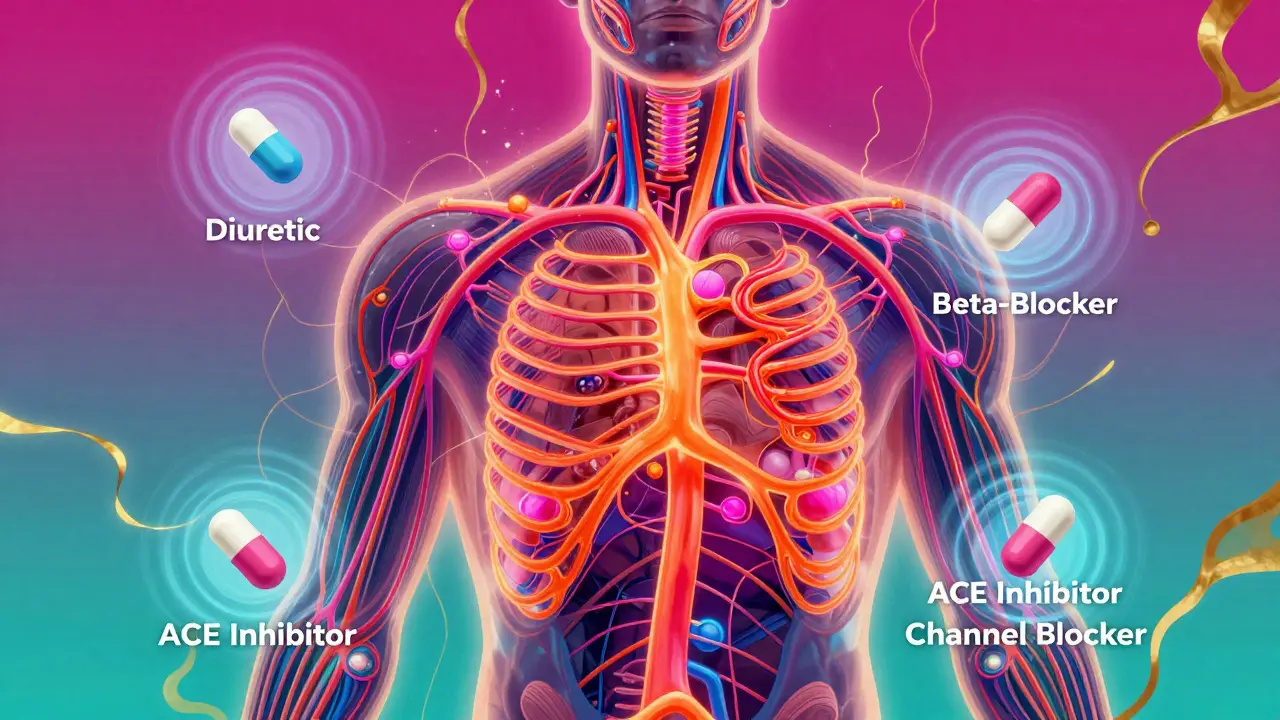
There’s no single way to lower blood pressure. Your body controls it through multiple systems: how much fluid is in your blood, how hard your heart pumps, how tight your arteries are. Each class of medication targets a different part of that system.
Diuretics, like hydrochlorothiazide, are often the first choice. They help your kidneys flush out extra salt and water. Less fluid in your blood means less pressure on your arteries. They’re cheap, effective, and backed by decades of data showing they reduce heart attacks and strokes.
Beta-blockers - such as metoprolol - slow your heart rate and reduce how hard your heart beats. They’re not usually first-line for pure hypertension anymore, but they’re essential if you’ve had a heart attack or have heart failure. They don’t just lower pressure; they protect your heart muscle.
ACE inhibitors like lisinopril and ARBs like losartan block a hormone called angiotensin II that tightens blood vessels. Both help relax arteries. The big difference? ACE inhibitors can cause a dry, annoying cough in up to 20% of people. ARBs don’t. That’s why many doctors switch patients from ACE inhibitors to ARBs if the cough starts.
Calcium channel blockers, such as amlodipine, stop calcium from entering heart and artery cells. This relaxes the arteries, lowering pressure. They work well for older adults and Black patients, who often respond better to these than to ACE inhibitors. Some types, like verapamil, also slow the heart rate - useful if you have an irregular heartbeat.
Other classes exist, but these four - diuretics, beta-blockers, ACE inhibitors, and calcium channel blockers - make up the backbone of treatment. Alpha-blockers, vasodilators, and others are usually added only when these don’t work enough.
Common Side Effects You Should Know
Side effects aren’t just annoying - they’re why so many people stop taking their meds. About half of patients quit within a year. Often, it’s not because the drug doesn’t work. It’s because they didn’t know what to expect.
With diuretics, you’ll need to pee more - especially at first. That’s normal. But they can also drop your potassium too low, causing muscle cramps or irregular heartbeat. Your doctor will likely check your blood levels every few months.
Beta-blockers can leave you feeling tired, cold, or sluggish. If you’re diabetic, they can hide the warning signs of low blood sugar - shaky hands, sweating, fast heartbeat. You’ll need to monitor your glucose more closely.
ACE inhibitors cause that dry cough in a lot of people. It’s not dangerous, but it’s persistent. If it’s keeping you up at night, ask about switching to an ARB. Both can raise potassium levels, which can be risky if you have kidney disease.
Calcium channel blockers like amlodipine often cause swollen ankles. It’s not dangerous, but it’s uncomfortable. Some people also get headaches or dizziness when they first start. Gingival hyperplasia - swollen gums - is rare but real. Good dental hygiene helps.
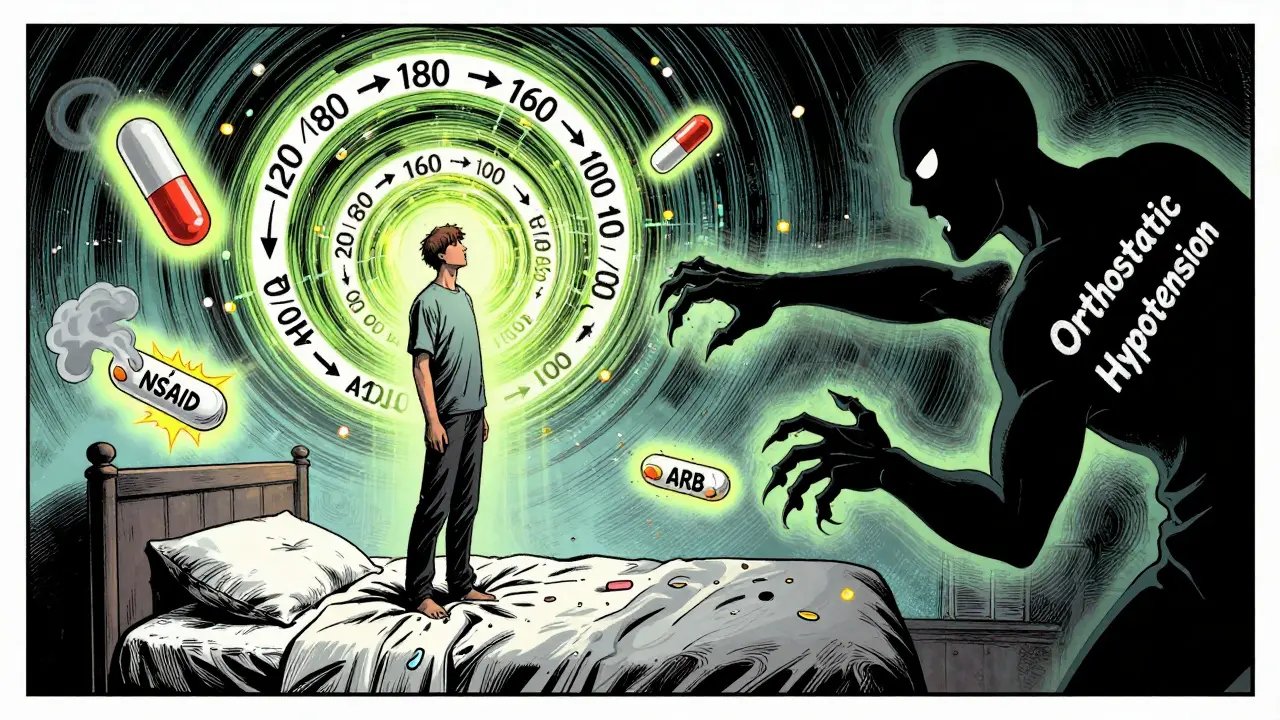
And then there’s orthostatic hypotension - that dizzy feeling when you stand up too fast. It’s common with alpha-blockers and some combinations of meds. Get up slowly. Sit on the edge of the bed for 30 seconds before standing. It’s a simple trick that prevents falls.
Safety First: What You Must Avoid
Not all drugs play nice together. Some combinations can do more harm than good.
Never take an ACE inhibitor and an ARB together. It sounds logical - two drugs blocking the same pathway - but studies show it increases the risk of kidney failure and dangerously high potassium without helping blood pressure any more. This combo is a red flag for doctors.
NSAIDs like ibuprofen or naproxen can cancel out the effect of your blood pressure meds. They also stress your kidneys. If you have high blood pressure and take these for arthritis or headaches, talk to your doctor. Acetaminophen is usually safer.
And if you’re pregnant - stop. ACE inhibitors, ARBs, and direct renin inhibitors can cause serious birth defects. If you’re planning pregnancy or think you might be pregnant, tell your doctor right away. Methyldopa and labetalol are the go-to options during pregnancy because they’ve been used safely for decades.
Older adults need extra care. Your body processes meds slower. A dose that’s fine for a 40-year-old might be too strong for a 75-year-old. Start low, go slow. Watch for dizziness, confusion, or falls. These aren’t normal aging - they’re signs your meds need adjusting.
Who Gets What? Personalizing Your Treatment
There’s no one-size-fits-all. Your age, race, and other conditions matter.
For most people without other health problems, guidelines recommend starting with a thiazide diuretic, a calcium channel blocker, or an ACE inhibitor/ARB. But for Black patients, studies show diuretics and calcium channel blockers work better than ACE inhibitors alone. That’s why doctors often pick those first.
If you have diabetes and kidney disease, ACE inhibitors or ARBs are the gold standard. They don’t just lower blood pressure - they protect your kidneys from damage. Same goes for people with heart failure. These drugs improve survival.
If you’ve had a heart attack, beta-blockers are critical. They reduce the chance of another one. If you have angina or an irregular heartbeat, calcium channel blockers like verapamil might be better than others.
And if your blood pressure is way too high - say, 160/100 or higher - you won’t get there with one pill. The 2025 American Heart Association guidelines say start with two drugs from different classes right away. One pill isn’t enough. Two are.
Combination Pills: Simpler, Smarter
Most people need more than one medication. Taking four pills a day is hard. That’s why combination pills exist.
Many come as a single tablet with a diuretic + ACE inhibitor, or a calcium channel blocker + ARB. You take one pill instead of two. It’s easier to remember. Studies show people stick with their meds better when they take fewer pills.
Common combos include lisinopril/hydrochlorothiazide, amlodipine/valsartan, or olmesartan/hydrochlorothiazide. Your doctor can prescribe these if you’re already on both drugs separately. It’s not a new treatment - just a smarter way to take it.
Monitoring and Adherence: The Real Challenge
Medication works only if you take it. And that’s the hard part.
Hypertension doesn’t hurt. You don’t feel better when you take your pill. So it’s easy to skip it - especially if you’re tired, traveling, or just forget. But skipping doses lets your pressure creep back up. That’s when damage happens.
Use a pill organizer. Set phone alarms. Link taking your pill to something you do every day - brushing your teeth, eating breakfast. Apps that track your blood pressure and remind you to take meds can improve adherence by 15-20%.
Your doctor should check your blood pressure every 2-4 weeks when you start or change meds. After that, every 3-6 months if you’re stable. Blood tests for potassium and kidney function are also routine, especially if you’re on ACE inhibitors, ARBs, or diuretics.
And if you’re having side effects - don’t just quit. Talk to your doctor. There’s almost always another option. Maybe a different dose. Maybe a different class. Maybe a combo pill. Giving up isn’t the answer. Adjusting is.
What’s Next? The Future of Blood Pressure Treatment
Research is moving fast. We’re starting to see how your genes affect how you respond to certain drugs. Some people metabolize beta-blockers slowly. Others barely respond to ACE inhibitors. In the next 5-10 years, genetic testing might help doctors pick your first pill - not guess, but know.
New drugs are being tested too. Endothelin blockers, for example, show promise for resistant hypertension. Digital tools - smart watches that track BP, apps that link to your pharmacy - are becoming part of standard care.
But the biggest breakthrough isn’t new. It’s consistency. Taking your meds daily. Getting your BP checked. Talking to your doctor when something feels off. That’s what saves lives.
Can I stop taking blood pressure medication if my numbers are normal?
No, not without talking to your doctor. Normal blood pressure on medication means the drug is working - not that your condition is cured. Stopping suddenly can cause your pressure to spike, sometimes dangerously. Some people can reduce or stop meds after major lifestyle changes, but only under medical supervision. Never quit on your own.
Which blood pressure medication has the least side effects?
There’s no single answer. Thiazide diuretics are generally well-tolerated but can cause low potassium. Calcium channel blockers like amlodipine are often easier for older adults but may cause ankle swelling. ARBs tend to have fewer side effects than ACE inhibitors because they don’t cause cough. The best medication is the one that works for you with the fewest side effects - and that’s different for everyone.
Are natural remedies safe to use with blood pressure meds?
Some can interfere. Garlic, hibiscus tea, and beetroot juice may lower BP slightly, but they’re not replacements. More dangerous are supplements like licorice root, which can raise BP, or St. John’s Wort, which can reduce the effectiveness of some meds. Always tell your doctor what supplements you’re taking - even if you think they’re "natural."
Why do I need to take two or more blood pressure pills?
Because high blood pressure is caused by multiple factors. One drug only targets one pathway. If your pressure is 160/100, one pill might lower it to 140/90 - still too high. Two drugs from different classes work together to hit multiple targets at once. That’s why most people need more than one. It’s not a failure - it’s standard care.
Can blood pressure meds cause weight gain?
Some can. Beta-blockers like metoprolol and older ones like atenolol may cause a small amount of weight gain - usually 1-2 kg - due to reduced metabolism or fluid retention. Calcium channel blockers can cause swelling in the legs, which adds temporary weight. Diuretics often cause weight loss because they remove fluid. If you notice unexplained weight gain, talk to your doctor. It’s not always the medication - but it’s worth checking.
What to Do If You’re Struggling
If your meds are making you feel worse - tired, dizzy, swollen - don’t suffer in silence. Write down your symptoms. Note when they happen. Bring them to your next appointment. Your doctor can adjust the dose, switch the class, or try a combo pill. There are over 50 approved blood pressure medications. You deserve one that works without ruining your day.
And if you’re forgetting to take them - use a pill box. Set a daily alarm. Link it to your coffee routine. Ask a family member to remind you. Adherence isn’t about willpower. It’s about systems. Make it easy. Your heart will thank you.
Caitlin Foster
December 28, 2025 AT 00:25So I’ve been on amlodipine for five years now, and honestly? The ankle swelling is the worst part. Not dangerous, sure, but imagine trying to fit into your favorite sneakers and they feel like tiny concrete boots. I started wearing compression socks and it’s a game-changer. Also, I take mine at night now - less dizziness in the morning. Side effects suck, but they’re manageable if you tweak the routine. Don’t just quit. Adjust.
Todd Scott
December 28, 2025 AT 09:55Let me tell you something most doctors won’t say out loud: the real reason we use diuretics first isn’t because they’re the best - it’s because they’re cheap and insurance covers them. The data is solid, yes, but if you’re a Black patient with salt-sensitive hypertension, calcium channel blockers might be the *actual* first-line choice, and yet so many still get hydrochlorothiazide by default. It’s not clinical wisdom - it’s systemic inertia. We need to move beyond one-size-fits-all guidelines and start treating patients, not algorithms.
Andrew Gurung
December 29, 2025 AT 00:19Ugh. Another ‘just take your pills’ lecture. 🙄 Meanwhile, Big Pharma is quietly funding studies that make ACE inhibitors look ‘safe’ while hiding the fact that 1 in 5 people get that cough and are told to ‘just endure it.’ And don’t get me started on combo pills - they’re not ‘smarter,’ they’re just a way to lock you into a brand-name regimen. Your doctor doesn’t care if you’re miserable. They just want your BP on their spreadsheet. Wake up.
Paula Alencar
December 30, 2025 AT 15:08It is of paramount importance to recognize that adherence to antihypertensive regimens is not merely a matter of personal responsibility - it is a complex interplay of socioeconomic factors, health literacy, and systemic access to care. Many individuals, particularly in underserved communities, face insurmountable barriers: lack of transportation to pharmacies, inability to afford copays, absence of reliable reminders, and cultural mistrust of medical institutions. To reduce medication non-adherence, we must address these root causes with compassion, policy reform, and community-based support systems - not merely with pill organizers and phone alarms. The human element cannot be outsourced to technology.
Nikki Thames
December 31, 2025 AT 08:55Have you ever considered that high blood pressure isn’t a disease at all - but a symptom of modern life? The processed foods, the chronic stress, the lack of sleep, the 12-hour workdays, the blue light poisoning your circadian rhythm? Medications are just Band-Aids on a wound caused by capitalism. They’re treating the symptom while the system keeps feeding you sugar, caffeine, and anxiety. You can take all the ARBs you want, but until you quit your job, move to the woods, and start growing your own kale, you’re just delaying the inevitable.
Chris Garcia
December 31, 2025 AT 13:39In my village in Nigeria, we used to treat hypertension with hibiscus tea, bitter leaf, and walking five miles to the market every day. Now, our youth take pills like candy, and no one walks anymore. I’m not saying we reject modern medicine - far from it. But we must remember that medicine without lifestyle is like a car without fuel. The pill lowers the number, but the walk, the meal, the quiet morning - those lower the *risk*. We must marry tradition with science, not replace one with the other.
James Bowers
January 2, 2026 AT 07:55It is a documented fact that the combination of ACE inhibitors and ARBs is contraindicated due to an increased incidence of hyperkalemia and acute kidney injury. The American College of Cardiology and the American Heart Association both explicitly warn against this practice in their 2023 clinical guidelines. Any practitioner who prescribes this combination is acting outside the standard of care and may be subject to malpractice liability. This is not a matter of opinion - it is medical fact.
Elizabeth Alvarez
January 3, 2026 AT 06:59Did you know that the FDA approved most of these drugs based on studies funded by pharmaceutical companies that buried negative results? The cough from ACE inhibitors? They knew about it for decades but called it ‘minor.’ The ankle swelling? Classified as ‘common but benign.’ And now they’re pushing combo pills to make you dependent on *their* brand. They’re not curing hypertension - they’re creating lifelong customers. Check the FDA’s own adverse event database. It’s terrifying. You’re not taking medicine. You’re participating in a corporate experiment.
dean du plessis
January 3, 2026 AT 23:48Kylie Robson
January 5, 2026 AT 02:27From a pharmacokinetic standpoint, the CYP2D6 polymorphism significantly influences the metabolism of beta-blockers such as metoprolol, resulting in poor metabolizers experiencing prolonged half-lives and increased risk of bradycardia, while ultra-rapid metabolizers may exhibit subtherapeutic concentrations. Consequently, genotype-guided dosing should be considered in all new prescriptions, particularly in patients with concomitant cardiac conditions. The current empirical dosing paradigm is antiquated and clinically suboptimal.
Will Neitzer
January 5, 2026 AT 14:19I appreciate the depth of this post - truly, it is one of the most comprehensive, evidence-based summaries of antihypertensive therapy I have encountered in recent years. The emphasis on personalized care, the acknowledgment of adherence challenges, and the recognition of structural inequities in prescribing patterns reflect a nuanced understanding of modern hypertension management. I would only add that the integration of digital health tools - such as validated home BP monitors synced to EHRs - must be prioritized in public health policy. Technology, when ethically deployed, can bridge the gap between clinical guidelines and real-world implementation.
Janice Holmes
January 7, 2026 AT 06:14Okay, but what if I told you… the real reason your BP won’t drop is because your house is haunted? I’m not joking. My cousin’s BP was 180/110 for two years. Pills? Nothing. Then they moved out of that 1920s Victorian with the ‘whispering walls’ and… poof. 120/80. No meds changed. Just… the house. I’m not saying you need a priest. But maybe… check your walls? 🕯️