When your liver starts acting up, it’s not always clear why. Fatigue, itchy skin, elevated liver enzymes - these symptoms show up in many conditions. But sometimes, they point to something more complex: an autoimmune overlap syndrome where two or more autoimmune liver diseases happen at once. The most common combinations involve Primary Biliary Cholangitis (PBC), Primary Sclerosing Cholangitis (PSC), and Autoimmune Hepatitis (AIH). These aren’t just random coincidences. They’re real, measurable, and often misunderstood.
What Exactly Is an Autoimmune Overlap Syndrome?
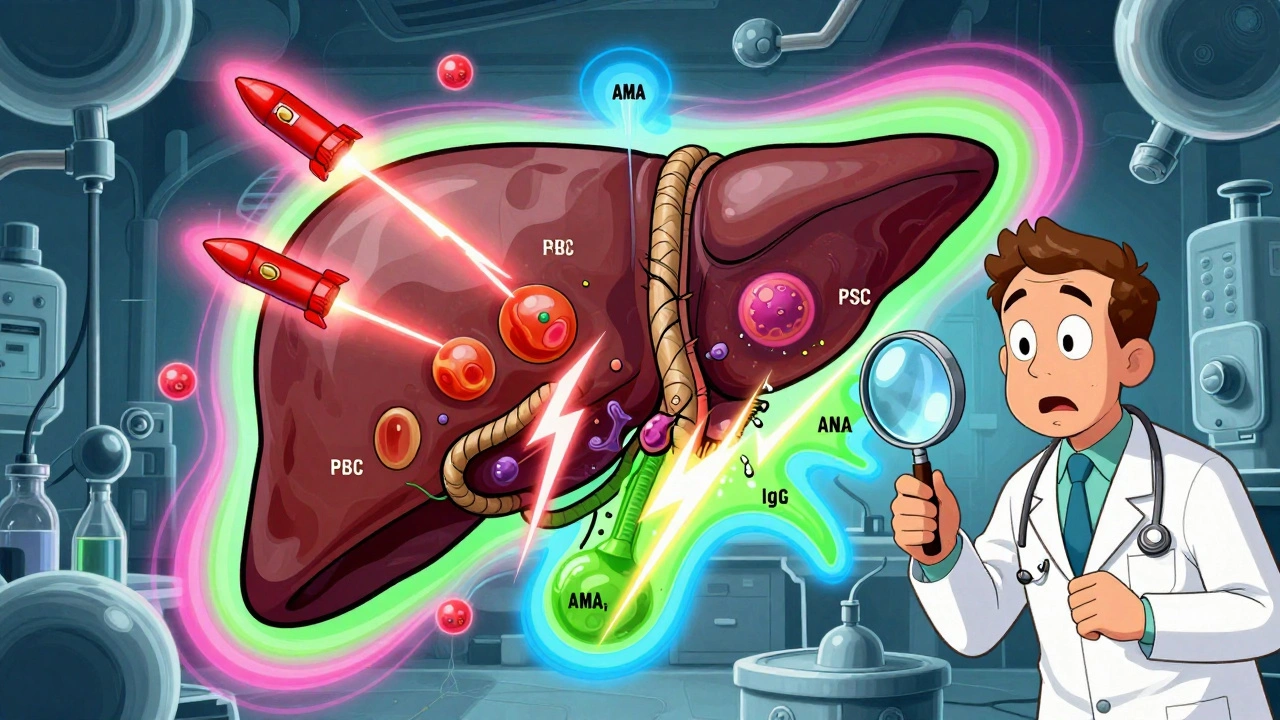
An overlap syndrome means your body’s immune system attacks your liver in more than one way at the same time. Imagine your immune system firing multiple types of missiles at different parts of the liver. In PBC, it targets the small bile ducts. In AIH, it attacks liver cells directly. In PSC, it causes scarring in the larger bile ducts. When these patterns show up together, doctors call it an overlap. The most frequently seen overlap is AIH-PBC. Studies show it affects 1% to 3% of people diagnosed with PBC, and up to 7% of those with AIH. Some larger studies even report numbers as high as 19% among PBC patients. That’s not rare. It’s common enough that every hepatologist should consider it. PBC-PSC overlap, however, is a different story. Despite a few scattered case reports, experts agree there’s no solid evidence this combination truly exists as a distinct condition. The features of PBC and PSC are too different - one affects tiny ducts deep in the liver, the other causes thick scarring in the main bile ducts. Most cases labeled as PBC-PSC overlap turn out to be misdiagnoses or two separate conditions occurring by chance.How Do You Tell Them Apart?
Each disease has its own fingerprint in blood tests and liver tissue. - AIH shows up with high ALT and AST (liver cell damage markers), elevated IgG, and autoantibodies like ANA or SMA. A liver biopsy will reveal interface hepatitis - inflammation right where liver cells meet the surrounding tissue. - PBC is marked by high ALP and GGT (cholestasis markers), elevated IgM, and the presence of anti-mitochondrial antibodies (AMA) in 90-95% of cases. The biopsy shows damage to small bile ducts, often with granulomas. - PSC also raises ALP and GGT, but unlike PBC, AMA is negative. It’s often linked to inflammatory bowel disease, especially ulcerative colitis. The telltale sign is a “beaded” appearance of bile ducts on MRCP or ERCP scans - think of a string of uneven beads. In an overlap, you see a mix. For example, someone with PBC might have normal AMA but also high IgG and interface hepatitis. That’s a red flag. Or a patient with AIH might suddenly develop elevated ALP - something that doesn’t fit the usual AIH profile. The diagnostic standard for AIH-PBC overlap is simple: meet at least two of the three diagnostic criteria for both diseases. That means: elevated ALP + positive AMA + biopsy findings for PBC, plus elevated IgG + autoantibodies + interface hepatitis for AIH. It’s not perfect, but it’s the best we have.Why Does This Matter for Treatment?
This isn’t just academic. Getting the diagnosis wrong can cost you years of health. PBC is treated with ursodeoxycholic acid (UDCA). It’s effective - slows progression, reduces transplant risk. But if you have AIH-PBC overlap, UDCA alone often isn’t enough. Around 30-40% of these patients don’t respond well to UDCA alone. Their liver enzymes keep climbing. Their fibrosis worsens. That’s where immunosuppressants come in. Steroids like prednisone and azathioprine are standard for AIH. In overlap cases, doctors often add them to UDCA. The goal isn’t to cure - no one has cured autoimmune liver disease yet - but to stop the damage before it turns to cirrhosis. One study followed 130 PBC patients. Nine percent met overlap criteria. Half of them needed combination therapy. Those who didn’t get it were more likely to progress to advanced scarring within five years. PSC is trickier. There’s no proven drug therapy. UDCA is sometimes used, but evidence is weak. In PSC-AIH overlap, immunosuppression can help - but only if the AIH component is strong. If you treat PSC like AIH, you might miss the bile duct scarring that leads to cancer risk.
Who Gets These Overlaps?
Women are far more likely to develop any of these conditions. PBC affects 90-95% women. AIH is 80% female. PSC is more balanced - about 60% male - but when PSC overlaps with AIH, the patient is still more likely to be female. Age matters too. PBC usually shows up between 40 and 60. AIH can strike younger - teens to 40s - or later in life. Overlap syndromes often appear in middle age, when someone has had mild liver enzyme elevations for years and suddenly gets worse. A 39-year-old man was diagnosed with PBC after routine bloodwork showed high ALP. He had no symptoms. But his IgG was sky-high, and his biopsy showed interface hepatitis. He didn’t fit PBC alone. He had AIH-PBC overlap. He started on UDCA, but within six months, his ALT didn’t drop. He was added to azathioprine. His enzymes normalized. He’s now monitored every six months.Why Misdiagnosis Is So Common
Many primary care doctors and even some gastroenterologists don’t test for AMA in patients with elevated liver enzymes. They see high ALT and assume it’s fatty liver or alcohol-related. Or they see high ALP and assume it’s gallstones. In community settings, misdiagnosis rates for autoimmune liver diseases hit 15-20%. For overlap syndromes, it’s even higher. Why? Because the symptoms are vague. Fatigue. Joint pain. Itchy skin. These show up in depression, menopause, thyroid issues, fibromyalgia. The key is knowing when to dig deeper. If someone has persistent cholestasis (high ALP) AND hepatocellular injury (high ALT), don’t stop at one diagnosis. Test for AMA, IgG, ANA, SMA. Do a biopsy if it’s unclear. Don’t assume it’s just one thing.What’s Next for Diagnosis and Treatment?
Researchers are working on better tools. New autoantibodies - like anti-sp100 and anti-gp210 - help diagnose AMA-negative PBC. These are found in 5-10% of cases where AMA is missing but the disease is still there. Large international groups - the International Autoimmune Hepatitis Group and EASL - are running multi-center studies to validate diagnostic criteria for overlap syndromes. Their goal: create a clear, reliable scoring system by 2025. We’re also learning that these diseases exist on a spectrum. Maybe AIH and PBC aren’t two separate diseases - maybe they’re different expressions of the same immune dysfunction. That’s why overlap syndromes aren’t anomalies. They’re clues.Long-Term Risks and Monitoring
Left untreated, 30-40% of overlap syndrome patients develop cirrhosis within 10 years. That’s similar to pure PBC or AIH. But the risk of liver cancer (hepatocellular carcinoma) might be higher in those with ongoing inflammation. That’s why lifelong monitoring is non-negotiable. Every 6-12 months: liver enzymes, IgG, ALP, AMA, ultrasound. Every 2-3 years, consider a FibroScan or MRI to check for scarring. If you’ve had an overlap diagnosis, you need a hepatologist - not just a general GI doctor. Liver transplant is still the last resort. But even after transplant, recurrence is possible. AIH can come back in the new liver. PBC can too. Patients with overlap syndromes need more careful post-transplant management.What You Should Do If You Suspect an Overlap
If you’ve been told you have PBC, AIH, or PSC - and your symptoms don’t match the expected course - ask these questions:- Have I been tested for AMA, ANA, SMA, and IgG?
- Was a liver biopsy done, and did it show interface hepatitis?
- Are my liver enzymes improving with treatment, or are they still climbing?
- Have I been referred to a liver specialist who sees autoimmune liver disease regularly?
Can you have PBC and PSC at the same time?
While there are rare case reports of patients showing features of both PBC and PSC, experts agree there is no clear evidence that a true PBC-PSC overlap syndrome exists. The two diseases affect different parts of the bile duct system and have distinct causes. Most cases labeled as overlap are likely misdiagnoses or two separate conditions occurring by chance.
Is AIH-PBC overlap rare?
No, it’s not rare. Studies show AIH-PBC overlap occurs in 1-3% of PBC patients and up to 7% of AIH patients. Some larger studies report rates as high as 19% among PBC patients. It’s one of the most common autoimmune liver disease overlaps.
Can you be treated with just UDCA if you have AIH-PBC overlap?
Sometimes, but not usually. About 30-40% of patients with AIH-PBC overlap don’t respond well to UDCA alone because the AIH component keeps attacking liver cells. Most need combination therapy - UDCA plus immunosuppressants like prednisone or azathioprine - to control both parts of the disease.
Do you need a liver biopsy to diagnose an overlap syndrome?
Not always, but it’s often necessary. PBC can be diagnosed without biopsy if AMA is positive and ALP is elevated. But for overlap syndromes, especially AIH-PBC, biopsy is critical to confirm interface hepatitis - the hallmark of AIH. Without it, you can’t confirm the second disease.
Can autoimmune overlap syndromes be cured?
No cure exists yet. But with proper treatment, progression can be slowed or stopped. Many patients live normal lifespans with regular monitoring and combination therapy. The goal isn’t cure - it’s preventing cirrhosis, liver failure, and cancer.
Evelyn Pastrana
December 10, 2025 AT 19:24So let me get this straight - we’re telling people their liver is having a full-on identity crisis and we’re still treating it like it’s just a bad case of too much pizza? 😅
Also, AMA-negative PBC? That’s like saying ‘I’m a cat’ but refusing to show the whiskers. We need better labels.
Lisa Whitesel
December 10, 2025 AT 20:33Doctors still don’t test for AMA routinely? That’s not negligence that’s criminal. People are getting misdiagnosed as fatty liver while their bile ducts turn to dust. No excuse. No mercy.
Simran Chettiar
December 11, 2025 AT 02:21It is fascinating to observe how the immune system, in its infinite complexity, does not adhere to the rigid categorical boundaries that human medicine insists upon. The convergence of PBC, AIH, and PSC suggests not merely coexistence but perhaps a deeper ontological unity - a single autoimmune spectrum manifesting in diverse phenotypes. We are not dealing with discrete diseases, but rather with the fractal expression of a dysregulated self-recognition mechanism. The biopsy, therefore, becomes not just a diagnostic tool, but a metaphysical witness to the body’s internal civil war.
Perhaps, in time, we shall abandon the language of disease and embrace the poetry of immune dysregulation.
Richard Eite
December 12, 2025 AT 23:05USA has the best liver docs in the world. If you’re getting misdiagnosed you’re not going to the right specialist. Stop blaming the system. Get better doctors. Or move to Canada and wait 6 months for a biopsy.
Katherine Chan
December 13, 2025 AT 11:11Okay but this is actually kind of hopeful? Like if we can catch this early and treat both parts? We’re not powerless here. People are surviving this. You don’t need to be cured to live well. Just listen to your body and push for the right tests. You got this 💪
Philippa Barraclough
December 15, 2025 AT 09:58The distinction between PBC-PSC overlap and coincidental comorbidity is methodologically fraught. The diagnostic criteria for each condition are based on distinct histopathological and serological markers, yet the overlap in clinical presentation - particularly in cholestatic enzyme elevation - creates significant diagnostic ambiguity. Moreover, the absence of longitudinal cohort studies specifically designed to evaluate the natural history of suspected PBC-PSC overlap renders any definitive conclusion regarding its existence premature. The current literature appears to conflate statistical coincidence with pathophysiological synergy, a tendency that risks both overdiagnosis and therapeutic misalignment. Further investigation with standardized phenotyping and imaging protocols is urgently required.
Tim Tinh
December 15, 2025 AT 21:46My cousin was diagnosed with PBC but her ALT stayed high - doc just said ‘wait and see.’ She went to a liver specialist on her own and they found AIH overlap. She’s on UDCA + azathioprine now and feels like a new person. Don’t let anyone brush this off. Ask for the AMA test. Ask for the biopsy. You’re worth it.
Ruth Witte
December 17, 2025 AT 14:59THIS. IS. EVERYTHING. 🙌
My mom had this and they almost missed it. Now she’s stable. Don’t ignore itchy skin. Don’t write off fatigue. Get the right tests. You’re not crazy. You’re not just tired. You’re fighting something real - and you’re not alone. 💖