Every time you take an antibiotic, you’re not just fighting an infection-you’re also wiping out trillions of good bacteria in your gut. Most people don’t realize that. But if you’ve ever had diarrhea after a course of amoxicillin or been told you’re at risk for C. difficile, you’ve felt the cost of overuse. Antibiotic stewardship isn’t a buzzword. It’s the quiet, science-backed movement changing how doctors prescribe-and how patients survive.
What Antibiotic Stewardship Really Means
Antibiotic stewardship means using antibiotics only when they’re truly needed, and when they are, using the right one, at the right dose, for the right amount of time. It’s not about avoiding antibiotics altogether. It’s about avoiding the wrong ones. The CDC defines it as the effort to measure and improve how antibiotics are prescribed by clinicians and used by patients. That’s it. Simple. Vital.In the U.S., more than 2.8 million antibiotic-resistant infections happen every year. Over 35,000 people die from them. And here’s the kicker: most of those infections started because someone got an antibiotic they didn’t need. A sore throat? Probably viral. A runny nose? Almost never bacterial. Yet, doctors still prescribe antibiotics for these in nearly half of outpatient visits.
Why Your Gut Is the First Casualty
Your gut is home to 38 trillion bacteria. Most of them are harmless-or even helpful. They digest fiber, make vitamins, train your immune system, and keep harmful bugs like Clostridioides difficile in check. When you take an antibiotic, especially a broad-spectrum one like ciprofloxacin or clindamycin, you don’t just kill the bad bacteria. You wipe out entire neighborhoods of good ones.That’s when C. difficile strikes. It’s a silent intruder that lies dormant in your gut until the good bacteria are gone. Then it multiplies like crazy, causing severe diarrhea, fever, and in worst cases, colon rupture. About 20% of people who take antibiotics get it. Each year in the U.S., C. difficile causes 223,900 infections and kills 12,800 people. And antibiotics are the number one risk factor.
It’s not just about hospital stays. Even a simple course of amoxicillin for a sinus infection can mess with your microbiome for months. Some studies show it takes over a year for gut bacteria to fully recover after just one round of antibiotics.
How Hospitals Are Fixing This
Hospitals with strong antibiotic stewardship programs have seen big wins. At a 444-bed hospital in Nebraska, a team of infectious disease doctors and pharmacists started doing what they call “handshake stewardship.” No forms. No approvals. Just walking into a doctor’s office, looking at the chart, and saying, “Hey, this patient has a viral infection. Let’s hold off on the antibiotic.”It sounds simple. But it works. Within a year, inappropriate antibiotic use dropped by 22%. C. difficile cases fell by 30%. And the hospital saved over $2 million a year-not from cutting drugs, but from avoiding complications, shorter stays, and fewer readmissions.
The CDC’s Core Elements framework spells out what works: leadership commitment, expert oversight, tracking antibiotic use, and education. Hospitals now track something called “days of therapy” per 1,000 patient days. That’s not a fancy term-it’s just how many days patients are on antibiotics. If that number drops, infection rates drop too.
What’s Happening Outside the Hospital
Most antibiotic use happens in doctor’s offices, not hospitals. And that’s where the biggest problems are. A 2022 CDC report found that 46% of antibiotic prescriptions for acute respiratory infections-like bronchitis, ear infections, and sinusitis-are unnecessary. Why? Because it’s easier to write a script than to explain why a virus doesn’t need antibiotics.But some clinics are changing that. One study put up posters in exam rooms that said: “I promise to only prescribe antibiotics when they’re truly needed.” Doctors who used them saw a 5.6% drop in inappropriate prescribing. That’s not huge-but in a system that prescribes billions of doses a year, it adds up to millions of fewer unnecessary antibiotics.
Another trick? Giving doctors real-time feedback. If Dr. Lee sees she’s prescribing 30% more antibiotics than her peers for sore throats, she starts asking: “Am I really helping?” Peer comparison works better than rules.
What You Can Do
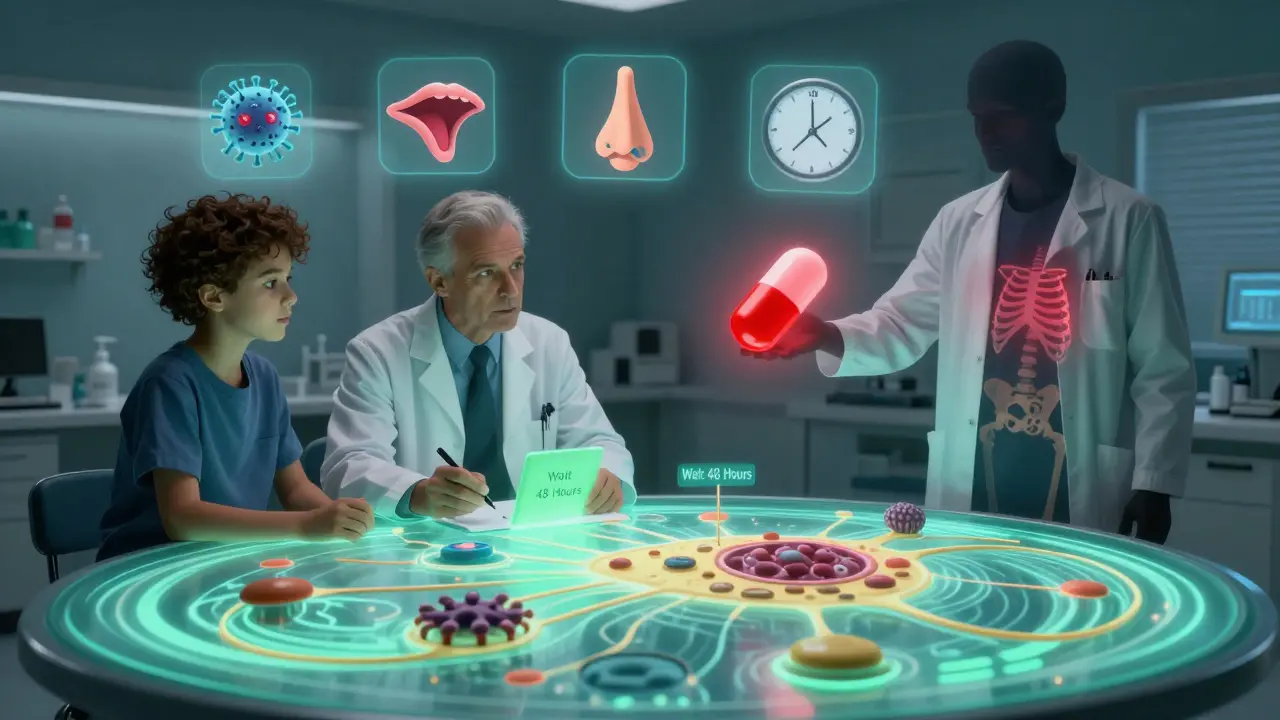
You don’t need to be a doctor to be part of the solution. Here’s what you can do:- Ask: “Is this infection bacterial?” If the answer is “I’m not sure,” push for a test. Rapid strep tests, flu swabs, and CRP blood tests can tell you if antibiotics are needed.
- Ask: “What happens if I wait?” Many infections, like ear infections in kids or sinus infections in adults, get better on their own. Waiting 48-72 hours is often safe-and saves your gut.
- Ask: “What’s the shortest course?” A 5-day course of amoxicillin is just as effective as a 10-day one for many infections. Shorter = less damage to your microbiome.
- Don’t pressure your doctor. If they say no antibiotics, don’t insist. You’re not being difficult-you’re being smart.
- After antibiotics, eat fermented foods: yogurt with live cultures, sauerkraut, kefir. They don’t “fix” your gut, but they help repopulate it faster.

The Bigger Picture: Resistance Is Already Here
Antibiotic resistance isn’t a future threat. It’s happening now. MRSA, drug-resistant tuberculosis, and carbapenem-resistant Enterobacteriaceae (CRE) are no longer rare. Some infections are now untreatable. In 2023, the WHO reported that 127 countries have national plans to fight resistance-and stewardship is at the heart of every one.When an antibiotic stops working, it’s not just that one drug that’s lost. It’s the whole pipeline. New antibiotics are expensive, slow to develop, and often less effective than older ones. We’re running out of options. Stewardship isn’t just about saving your gut-it’s about saving the last line of defense for when you really need it.
What’s Next
The future of stewardship is smarter, faster, and more precise. AI tools are being tested in hospitals to analyze patient data and suggest the best antibiotic within seconds. Some systems now flag prescriptions that don’t match guidelines before they’re even written. That’s not science fiction-it’s happening in teaching hospitals right now.And pediatric guidelines are catching up. The American Academy of Pediatrics updated its advice in 2020, showing that for ear infections in kids over 2, watchful waiting is often better than antibiotics. For strep throat, rapid tests cut down on overprescribing by 40%.
By 2025, the CDC projects that widespread stewardship could prevent 130,000 C. difficile infections and save 10,000 lives in the U.S. alone. That’s not a guess. It’s based on data from hundreds of hospitals that have already done it.
This isn’t about being anti-antibiotic. It’s about being pro-smart. Every antibiotic you don’t take is one less chance for resistance to grow. One less chance for your gut to collapse. One more drug left for when you really need it.

Arjun Seth
January 15, 2026 AT 20:55Everyone just takes antibiotics like candy, and then wonders why they’re always sick. It’s not rocket science. If your nose runs for three days, you don’t need a prescription-you need a nap. And yet, people demand them like they’re owed something. I’ve seen moms cry because the doctor didn’t give them a pill for a cold. What are we raising? A generation of medical zombies?
Jaspreet Kaur Chana
January 16, 2026 AT 22:57Let me tell you something from my village in Punjab-we never had antibiotics growing up, and we were healthier. My grandmother used turmeric paste for every cut, ginger tea for every cough, and honey for every sore throat. We didn’t have fancy labs or doctors, but we didn’t have C. diff either. Now kids in cities get antibiotics for sniffles, and their guts are ruined before they’re ten. We lost something real when we traded wisdom for pills. It’s not just medicine-it’s culture. And we’re throwing it away like trash.
Haley Graves
January 17, 2026 AT 18:54As a nurse who’s seen patients crash from C. diff, I can tell you this: the system is broken, but it’s fixable. Doctors aren’t evil-they’re overwhelmed. Patients aren’t stupid-they’re scared. What works is education, not guilt. We need more nurse-led stewardship teams in clinics, not just in hospitals. And we need to stop treating patients like adversaries. If you walk in with a sore throat and leave with a plan and a pamphlet, you’re more likely to trust the system next time.
Gloria Montero Puertas
January 18, 2026 AT 13:12It’s astonishing how little the public understands microbiology. The gut isn’t some mystical garden-it’s an ecosystem, and antibiotics are like napalm. And yet, people still believe in ‘detox teas’ and ‘probiotic gummies’ as magic bullets. The fact that someone thinks yogurt fixes antibiotic damage shows how deeply science denial has permeated wellness culture. This isn’t about ‘smart prescribing’-it’s about basic biology education. We need mandatory public health literacy courses. Starting in middle school. No exceptions.
Tom Doan
January 18, 2026 AT 20:52It’s ironic that we’ve engineered antibiotics to kill bacteria, yet we’ve failed to engineer a cultural response to their overuse. We treat medicine like a commodity, not a privilege. The fact that a 22% reduction in inappropriate prescribing leads to a 30% drop in C. diff cases suggests that the problem isn’t scarcity-it’s behavior. And behavior is shaped by incentives. So why are doctors still rewarded for volume, not precision? The system is designed to fail. And we’re all just playing our parts.
Annie Choi
January 20, 2026 AT 19:12Microbiome collapse is the silent pandemic. We’re not just losing antibiotics-we’re losing immune resilience. I work in pediatric oncology. Kids who’ve had multiple rounds of broad-spectrum antibiotics before age five have way higher rates of secondary infections. It’s not correlation-it’s causation. We need to treat the microbiome like an organ. And we need to stop calling it ‘gut health’ like it’s a yoga trend. It’s physiology. It’s survival.
Jan Hess
January 20, 2026 AT 23:45I used to get antibiotics for every cold until I got C. diff after a sinus infection. Took me six months to feel normal again. Now I ask for tests. I wait 48 hours. I eat sauerkraut. I don’t pressure my doctor. It’s not hard. It’s just different. And honestly? I feel better than I did in years. My gut isn’t perfect but it’s mine again. You don’t need a PhD to do this. You just need to stop trusting the pill bottle over your own body.
Dan Mack
January 21, 2026 AT 11:55Big Pharma is behind this. They don’t want you to know antibiotics can be avoided. They make billions from overprescribing. And the CDC? They’re funded by drug companies. Look at the data-every ‘study’ says antibiotics are safe. But the real data? The one they don’t publish? It shows gut damage lasts years. And the new AI tools? They’re not to help you-they’re to make doctors faster so they can prescribe more. This isn’t stewardship. It’s a marketing scheme with a lab coat.
Amy Vickberg
January 23, 2026 AT 04:16I’ve been on both sides-patient and caregiver. My mom nearly died from C. diff after a simple dental antibiotic. That’s when I learned to ask the three questions in the article. And guess what? Doctors appreciate it. They’re tired of guessing too. When you come in calm, informed, and willing to wait, they feel supported-not challenged. This isn’t about being anti-medical. It’s about being pro-wellness. And that’s something we can all get behind.
Ayush Pareek
January 24, 2026 AT 17:20My uncle in Delhi used to say, ‘If your body can’t fight it, maybe it wasn’t meant to be fought.’ He never took antibiotics unless he was in the hospital. He lived to 92. I’m not saying avoid medicine-but don’t rush to it. Wait. Observe. Listen to your body. That’s the real wisdom. We’ve forgotten how to be patients. We’ve become consumers. And that’s the problem.
Sarah Mailloux
January 24, 2026 AT 23:44After my third round of antibiotics, I started eating kimchi every day. No joke. My bloating vanished. My energy came back. I didn’t ‘fix’ my gut-I helped it heal. And I stopped asking for pills. My doctor said I was the best patient he’d had in years. Funny how that works.
Nilesh Khedekar
January 25, 2026 AT 04:06You think this is about antibiotics? Nah. It’s about control. The system wants you dependent. Pills. Tests. Follow-ups. Bills. If you heal yourself with food and time, who profits? The real enemy isn’t C. diff-it’s the healthcare industrial complex. They don’t want you healthy. They want you recurring. And you’re letting them win by not asking questions. Stop trusting the white coat. Start trusting your gut.