Many people assume that generic medications are just cheaper copies of brand-name drugs - and in most ways, they’re right. The same active ingredient, same dosage, same effect. But here’s something most patients don’t know: generic medications can trigger allergic reactions that brand-name versions never did. And it’s not because of the medicine itself. It’s because of what’s hiding in the pills - the fillers, dyes, and preservatives that aren’t required to match the brand-name version.
Why generics can cause reactions brand names don’t
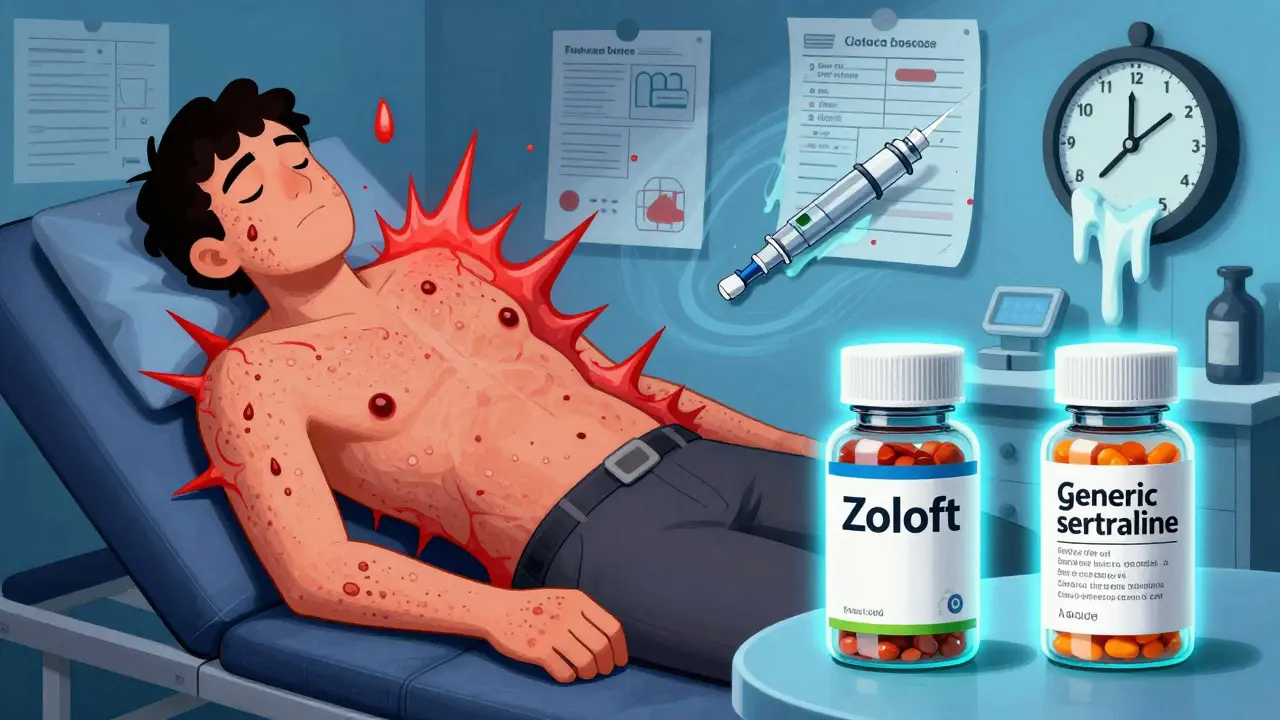
Generic drugs must contain the same active ingredient as the brand-name drug, and they must work the same way in your body. That’s regulated by the FDA. But when it comes to the other ingredients - the ones that hold the pill together, give it color, or help it dissolve - there’s no such requirement. That’s where problems start. Take lactose, for example. About 28% of oral generic medications contain it. If you’re lactose intolerant, that’s not just a stomachache - it can trigger hives, swelling, or worse. Gluten shows up in 12% of generics. For someone with celiac disease, even a tiny amount can cause a serious immune response. Then there’s tartrazine (Yellow No. 5), a dye used in 15% of liquid generics. It’s linked to allergic reactions in sensitive people, including asthma flare-ups and hives. And in rare cases, injectable generics contain peanut oil - a deadly risk for those with peanut allergies. A 2021 study in the Journal of Allergy and Clinical Immunology found that 7.3% of patients who thought they were allergic to a drug were actually reacting to these inactive ingredients in the generic version. One patient in California had no issues with brand-name sertraline (Zoloft) but broke out in hives within 30 minutes of switching to the generic. Turns out, the generic used tartrazine. The brand didn’t.What the symptoms look like - and when they’re dangerous
Reactions to generics can range from mild to life-threatening. Most start with skin symptoms: itching, redness, hives, or a rash. About 68% of mild reactions involve a rash. Hives show up in 42% of cases. These might seem like a nuisance, but they’re your body’s warning sign. Moderate reactions mean more than one system is involved. Think hives + nausea, or swelling + wheezing. Facial swelling, especially around the lips or tongue, is a red flag. So is trouble breathing, a tight throat, or vomiting that doesn’t go away after a couple of hours. These aren’t just side effects - they’re signs your immune system is overreacting. Severe reactions - anaphylaxis - are rare but deadly. They happen in about 0.02% to 0.04% of generic drug doses. But when they do, they strike fast. Eighty-seven percent of anaphylaxis cases involve throat tightness. Seventy-eight percent cause a sudden drop in blood pressure. Ninety-two percent lead to severe breathing trouble. And 43% of these reactions begin within 15 minutes of taking the pill.When to call 911 - not wait and see
If you’re taking a generic medication and you feel any of these, don’t wait. Don’t take an antihistamine and hope it goes away. Call emergency services immediately:- Difficulty breathing, wheezing, or stridor (a high-pitched sound when you breathe)
- Swelling of the throat, tongue, or lips
- Sudden dizziness, fainting, or a rapid, weak pulse
- Low blood pressure - feeling like you’re going to pass out
- Two or more symptoms at once - like hives + vomiting + trouble breathing
When to call your doctor - even if it seems minor
Not every reaction is an emergency. But even mild ones need attention. If you develop hives that last more than six hours, swelling that doesn’t go down after a few hours, or stomach symptoms that stick around for more than two hours, contact your doctor within 24 hours. Don’t brush it off as “just a bad reaction.” Why? Because 65% of people who have a mild reaction to a generic medication will have a worse one the next time they take it. That’s not luck. That’s how the immune system works. Once it’s sensitized, it reacts faster and harder. Your doctor needs to know exactly what you took - not just “generic sertraline,” but which brand, which batch, and what the pill looked like. That’s because different generic manufacturers use different inactive ingredients. One version might be safe; another might not.What you can do to protect yourself
You don’t have to live in fear of generics. But you do need to be smart.- Ask your pharmacist - every time you fill a generic prescription - what inactive ingredients are in it. They have access to the FDA’s Inactive Ingredient Database and can tell you if it contains lactose, gluten, dyes, or peanut oil.
- Keep a “medication allergy passport”. Write down every ingredient you’re allergic to - not just the drug name, but the filler. For example: “Allergic to tartrazine (Yellow No. 5) in generic sertraline.” Show this to every doctor and pharmacist.
- Request dye-free, gluten-free, or lactose-free versions. About 38% of major generic manufacturers now offer these options. They’re not always advertised, but they exist. Ask.
- Get tested. If you’ve had a reaction, see an allergist. Many people are mislabeled as allergic to a drug when they’re really allergic to an inactive ingredient. Formal testing can clear you for future use of the active drug - even if you had a bad reaction to a generic.


Aysha Siera
January 16, 2026 AT 18:29They’re hiding poison in your pills and calling it medicine. The FDA? A puppet. Big Pharma owns them. You think they care if you break out in hives? No. They care about profit. Tartrazine. Lactose. Peanut oil. All legal. All hidden. You’re not allergic to the drug-you’re allergic to the system.
rachel bellet
January 17, 2026 AT 18:01Statistically, the incidence of non-active ingredient-mediated hypersensitivity is significantly underreported due to diagnostic overshadowing. The FDA’s inactive ingredient database lacks granular traceability, and pharmacovigilance systems are not structured to correlate batch-level excipient variance with adverse event clusters. This is a pharmacokinetic blind spot with clinical implications.
Emma #########
January 19, 2026 AT 02:32I had a rash after switching generics and just thought it was stress. I didn’t connect it until I read this. Thank you for putting this out there. I’m going to my pharmacist tomorrow to ask about the fillers.
Selina Warren
January 20, 2026 AT 14:33This is why we need to stop treating health like a spreadsheet. Your body isn’t a cost-center. If a pill makes you break out in hives, it doesn’t matter if it’s 87% cheaper. You’re not a number. You’re a person. And your life isn’t a bargain bin item.
Stacey Marsengill
January 20, 2026 AT 16:07Of course it’s the fillers. I’ve been saying this for years. People think if it’s ‘generic’ it’s just a cheaper version of the same thing-but no. It’s a different recipe. Like ordering a burger and getting the same patty but with expired buns, moldy lettuce, and someone’s sweat on the sauce. You don’t get sick from the beef-you get sick from the trash they put around it.
I once took a generic for anxiety and broke out in hives from my neck to my knees. No one believed me until I looked up the pill’s ingredients. Tartrazine. Same drug. Different poison. I switched back to brand. No more itching. No more panic. Just peace.
And now? I keep a little card in my wallet. ‘Allergic to Yellow No. 5, lactose, gluten, and corporate negligence.’ I hand it to every pharmacist. Some laugh. One cried. I didn’t know whether to feel validated or furious.
Nishant Sonuley
January 21, 2026 AT 05:39Hey, I’m from India and we get generics everywhere-sometimes even from unregulated factories. But here’s the thing: in places like ours, people don’t have the luxury of asking about fillers. They take what’s available. So yes, this is important for those who can choose-but what about the millions who can’t? Maybe we need a global standard, not just a US fix.
Also, I’ve seen pharmacists in Delhi just hand out pills without even checking the name. One guy gave me a pill that looked like a candy. No label. Just a color. I asked what it was. He shrugged. ‘It’s medicine.’
Robert Davis
January 23, 2026 AT 02:32Look, I’m not saying the FDA is perfect, but you’re overreacting. Most people don’t have reactions. The odds are tiny. If you’re that sensitive, maybe you should just stick with brand-name drugs and pay the extra $50 a month. It’s not rocket science.
Also, peanut oil in injectables? That’s not even a thing in most generics. You’re spreading fear based on one outlier case.
Andrew Short
January 24, 2026 AT 02:42Oh, here we go. Another ‘I’m special because I’m allergic to dyes’ narrative. Wake up. If you can’t handle the fillers, you’re not ‘sick’-you’re just weak. The body adapts. You don’t get to demand custom pills because you’re too fragile to handle a little lactose.
And let’s be real-this isn’t about safety. It’s about entitlement. You want to pay less? Fine. But if you want perfect, go live in Switzerland and pay $300 for a pill. Don’t cry because you chose the cheaper option and now your skin itches.
Robert Cassidy
January 25, 2026 AT 12:38They’re letting foreign factories make our pills. China. India. Who knows where. No oversight. No inspections. You think your ‘generic’ sertraline was made in a sterile lab? Nah. It was made in a warehouse with no AC, rats running through, and a guy named Li who didn’t wash his hands after using the bathroom.
And you want to know why they use peanut oil? Because it’s cheap. And they don’t care if you die. They don’t care if your kid has anaphylaxis. They’re shipping pills to America like they’re shipping cheap socks. This isn’t healthcare. It’s colonialism with a pharmacy label.
And don’t tell me to ‘ask my pharmacist.’ Most of them are just glorified cashiers. They don’t know what’s in the pills. They scan and send. That’s it.
Naomi Keyes
January 27, 2026 AT 07:29Per the FDA’s Guidance for Industry on Inactive Ingredients, Section 4.2: ‘While excipients are not required to be bioequivalent to those in the reference listed drug, manufacturers are encouraged to disclose potential allergens.’ Yet, per the 2022 FDA Adverse Event Reporting System (FAERS) data, only 12% of generic submissions include allergen labeling in the product monograph. This is a systemic regulatory gap requiring immediate policy intervention.
Furthermore, the National Library of Medicine’s DailyMed database contains 89% of active ingredient data but only 31% of excipient-level allergen data. This is not a patient failure-it is a documentation failure.
Andrew McLarren
January 28, 2026 AT 09:10I appreciate the depth of this post. It’s rare to see such a nuanced discussion on a topic that affects so many silently. I work in a rural clinic, and I’ve seen patients come in with rashes, thinking they’re allergic to the medication-only to discover it was the dye. I’ve started asking patients to bring in the pill bottle or take a photo of the pill. It’s changed how we diagnose.
Thank you for emphasizing the importance of the ‘medication allergy passport.’ I’m going to make a template and hand it out to every patient with a history of reactions. This is the kind of information that saves lives.
Eric Gebeke
January 30, 2026 AT 00:46Wow. Just… wow. I thought I was just being dramatic when I broke out in hives after switching to generic sertraline. I even felt guilty for complaining. But now I realize-I wasn’t weak. I was right. And now I’m going to make sure every doctor, every pharmacist, every nurse knows what happened. Because someone else shouldn’t have to suffer because no one was paying attention.