ACE Inhibitor & ARB Interaction Checker
Select your medication and click "Check Risk" to see potential side effects and recommendations.
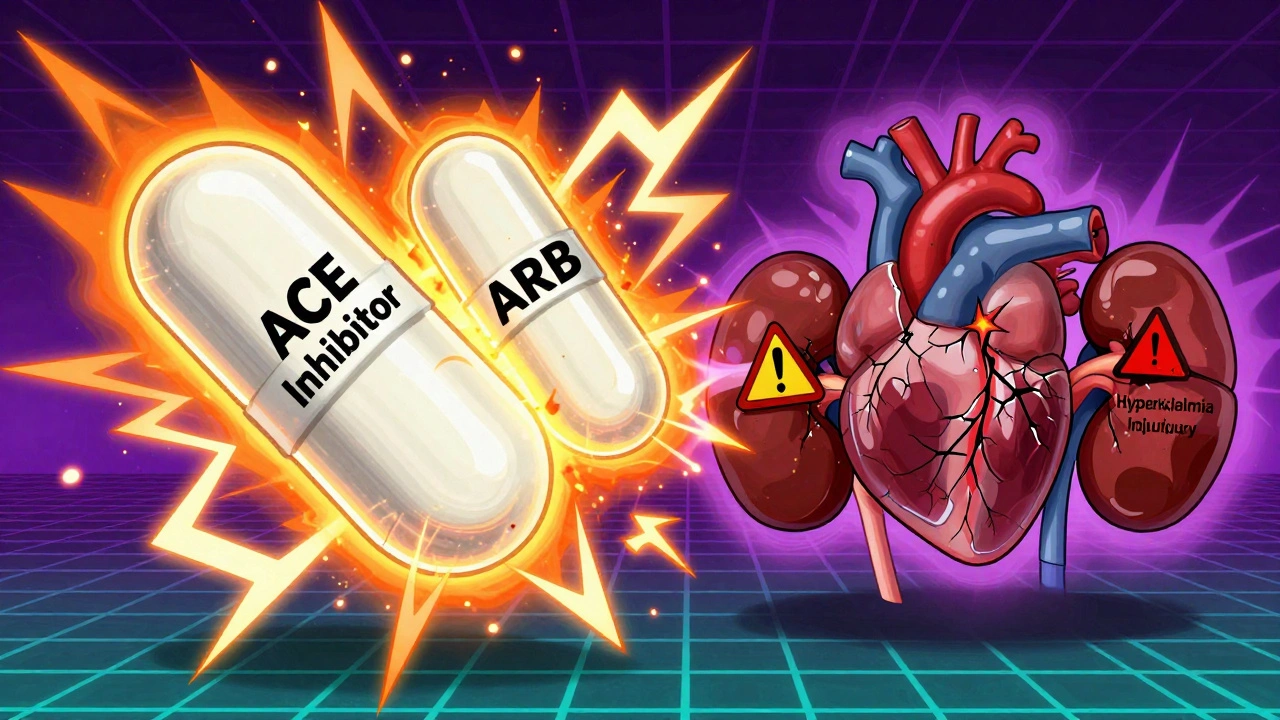
Many people take ACE inhibitors or ARBs to manage high blood pressure, heart failure, or kidney disease. These drugs work in similar ways-both target the renin-angiotensin system-but they’re not the same. Mixing them together sounds like it should make things better, right? More power to fight high blood pressure. But here’s the truth: combining ACE inhibitors and ARBs is dangerous for most people. It doesn’t give you better results. It just ups your risk of serious side effects.
How ACE Inhibitors and ARBs Work
ACE inhibitors like lisinopril, enalapril, and ramipril stop your body from making angiotensin II, a chemical that tightens blood vessels and raises blood pressure. They do this by blocking the enzyme that turns angiotensin I into angiotensin II. Less angiotensin II means relaxed blood vessels, lower blood pressure, and less strain on your heart and kidneys.
ARBs-like losartan, valsartan, and irbesartan-work differently. Instead of stopping angiotensin II from being made, they block its receptors. Think of it like putting a lock on the door angiotensin II tries to open. Even if angiotensin II is still around, it can’t do its job. This is why ARBs are often used when someone can’t tolerate ACE inhibitors.
One big difference? ACE inhibitors cause a buildup of bradykinin, a substance that can trigger a dry, hacking cough in 10-15% of users. ARBs don’t do this. That’s why about 1 in 6 people switch from an ACE inhibitor to an ARB-not because the first one didn’t work, but because they couldn’t stand the cough.
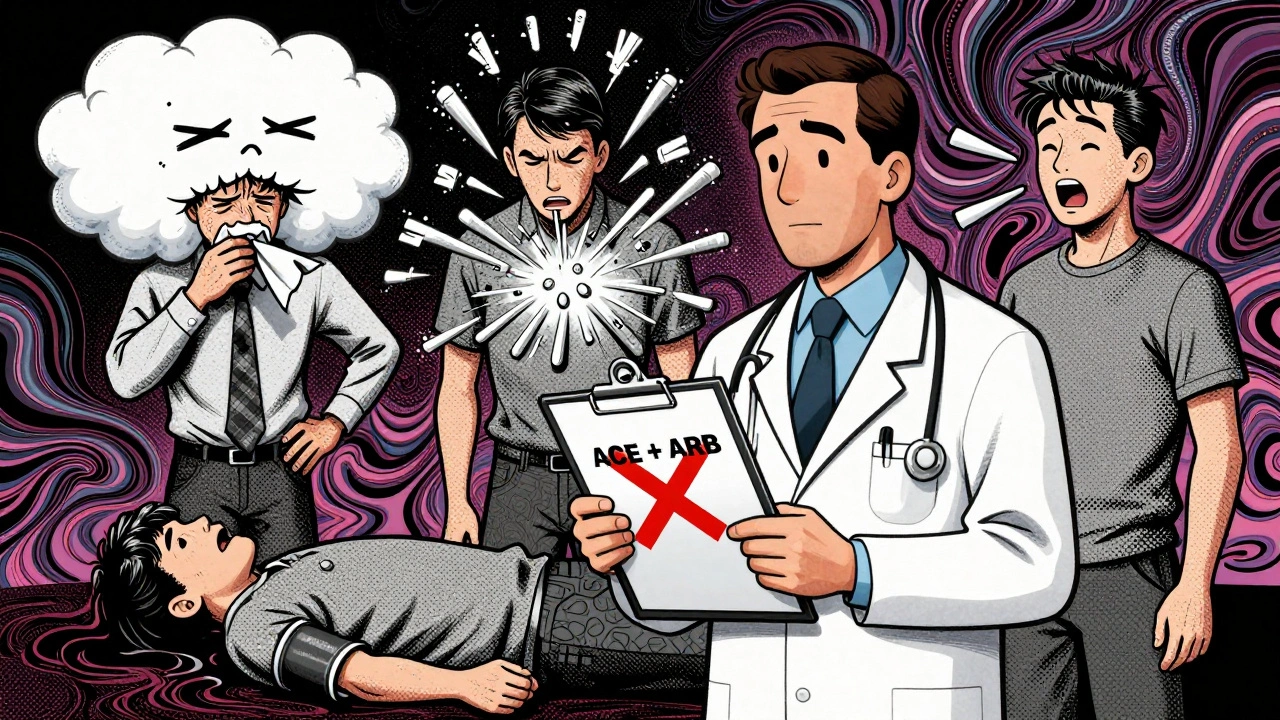
Why You Shouldn’t Mix Them
The idea of combining ACE inhibitors and ARBs seems logical: double the blockade, better results. But studies have shown this doesn’t work that way. The ONTARGET trial in 2008 followed over 25,000 high-risk patients. Half got ramipril (an ACE inhibitor). Half got telmisartan (an ARB). A third group got both. The combo group had no fewer heart attacks, strokes, or deaths. But they had way more problems.
Here’s what happened:
- Renal failure requiring dialysis went from 1% to 2.3%
- Hyperkalemia (dangerously high potassium) jumped from 2.5% to 5.5%
- Low blood pressure, dizziness, and kidney injury increased by nearly 80%
The VA NEPHRON-D trial in 2018 confirmed this. In diabetic patients with kidney disease, adding an ARB to an ACE inhibitor didn’t slow kidney decline. Instead, it increased serious side effects by 27%. That’s not a trade-off worth making.
Today, the American Heart Association, the American College of Cardiology, and the European Society of Cardiology all say: don’t combine ACE inhibitors and ARBs. Not for hypertension. Not for diabetic kidney disease. Not unless you’re in a research study.
When Cross-Reactivity Matters
Even if you’re not taking both drugs at once, cross-reactivity can still be a problem. About 1 in 100 people who get angioedema (swelling of the face, lips, or throat) on an ACE inhibitor will also get it on an ARB. It’s rare-0.1% to 0.2%-but it’s real. If you’ve had angioedema on lisinopril, switching to losartan isn’t a safe fix.
Also, if you’ve had a severe cough on an ACE inhibitor, you’re more likely to switch to an ARB. But don’t assume the ARB is a perfect replacement. Some people still feel off-fatigue, dizziness, or even mild kidney changes. That’s because both drugs affect the same system. Your body doesn’t suddenly forget how to react.
Side Effects You Can’t Ignore
Both classes of drugs can raise potassium and hurt kidney function, especially in older adults or those with existing kidney disease. Here’s what you need to watch for:
- High potassium (hyperkalemia): Both drugs reduce aldosterone, which tells your kidneys to dump potassium. Without it, potassium builds up. Levels above 5.5 mmol/L can cause dangerous heart rhythms.
- Acute kidney injury: Especially if you’re dehydrated, on diuretics, or have narrowed kidney arteries. Your kidneys rely on angiotensin II to keep blood flowing through them. Block that, and filtration drops fast.
- Low blood pressure: Dizziness, fainting, or falls-especially when standing up. This is common when starting or increasing the dose.
That’s why doctors check your blood work 1-2 weeks after starting or changing the dose. Then every 3 months. If your creatinine jumps more than 30% or your potassium goes above 5.0, you need to adjust the treatment.
What to Do Instead
If your blood pressure isn’t controlled on one drug, don’t add the other. Here’s what works better:
- Add a diuretic: Hydrochlorothiazide or chlorthalidone helps flush out extra fluid and lowers potassium slightly.
- Add a calcium channel blocker: Amlodipine is often paired with an ACE inhibitor or ARB for better control.
- Try a mineralocorticoid receptor antagonist: Spironolactone (12.5-25 mg daily) reduces proteinuria and protects the heart without the risks of dual RAS blockade.
- Switch to an ARNI: Sacubitril/valsartan (Entresto) is now first-line for heart failure with reduced ejection fraction. It blocks the bad effects of angiotensin II while boosting protective peptides. It’s not a combo of ACE + ARB-it’s a new kind of drug.
For people with heavy proteinuria (>1 gram/day) who aren’t diabetic, some nephrologists still consider adding an ARB to an ACE inhibitor. But this is rare. It requires weekly blood tests, no NSAIDs, and no salt substitutes. Most doctors won’t touch it unless everything else has failed.
Real-World Experience
Dr. Lisa Chen, a nephrologist at Massachusetts General Hospital, stopped combination therapy in 87% of her 215 diabetic kidney disease patients. Why? Their potassium levels rose an average of 0.8 mmol/L. Their kidney function dropped by 15% in just a few months. No one got better. Some got worse.
On Reddit, medical students report seeing hyperkalemia hospitalizations from this combo more than once during rotations. One resident wrote: “I saw a 62-year-old man on lisinopril and losartan come in with a potassium of 6.8. He needed emergency dialysis. He didn’t know he was on both.”
Meanwhile, the few cases where the combo seemed to help-like in rare kidney diseases such as focal segmental glomerulosclerosis-require extreme monitoring. Weekly labs. No NSAIDs. No potassium-rich foods. It’s not a lifestyle you want.
Switching Safely
If you need to switch from an ACE inhibitor to an ARB, don’t just swap them on the same day. The Cleveland Clinic recommends a 4-week washout period. Why? Because ACE inhibitors can linger in your system, and their effects on angiotensin II levels take time to reverse. Jumping straight to an ARB can cause a sudden drop in blood pressure or kidney function.
But here’s the catch: only 42% of doctors follow this rule. That’s a problem. If you’re switching, ask your doctor for a clear plan. Don’t assume it’s automatic.
What’s Next?
The future of RAS blockade isn’t in combining ACE inhibitors and ARBs. It’s in newer drugs. ARNIs like Entresto are already replacing them in heart failure. SGLT2 inhibitors like dapagliflozin and empagliflozin-originally diabetes drugs-are now proven to protect kidneys and hearts in people with or without diabetes. They’re safer, easier to use, and don’t raise potassium.
The FINE-REWIND trial, running from 2024 to 2028, is testing ultra-low-dose ACE + ARB combinations. But even the researchers don’t expect this to become standard. They’re just exploring if tiny doses might help without the risks.
By 2028, experts predict less than 1% of RAS blocker prescriptions will involve combining ACE inhibitors and ARBs. That’s because the data is clear: the risks outweigh the benefits. Every major guideline says so. Every real-world study confirms it.
If you’re on one of these drugs and your blood pressure isn’t where it should be, talk to your doctor about safer ways to adjust. Don’t assume adding another RAS blocker is the answer. It’s not. It’s a trap.
Can I take an ACE inhibitor and ARB together for better blood pressure control?
No. Combining an ACE inhibitor with an ARB does not improve survival, heart attack prevention, or long-term kidney outcomes. It doubles the risk of dangerously high potassium levels and increases the chance of acute kidney injury. Major guidelines from the American Heart Association and American College of Cardiology strongly advise against this combination outside of clinical trials.
Why do some people switch from ACE inhibitors to ARBs?
The most common reason is a persistent dry cough, which affects 10-15% of people on ACE inhibitors. This cough is caused by bradykinin buildup, a side effect unique to ACE inhibitors. ARBs don’t cause this, so they’re a preferred alternative for patients who can’t tolerate the cough. However, ARBs are not a perfect substitute-some people still experience dizziness or kidney changes.
Is it safe to take an ARB if I had angioedema on an ACE inhibitor?
Not usually. Angioedema (swelling of the face, lips, or throat) occurs in about 0.1-0.7% of people on ACE inhibitors. While ARBs have a lower risk (0.1-0.2%), there is still cross-reactivity. About 1 in 10 people who had angioedema on an ACE inhibitor will have it again on an ARB. If you’ve had this reaction, avoid ARBs and discuss safer alternatives like calcium channel blockers or diuretics with your doctor.
How often should I get blood tests if I’m on an ACE inhibitor or ARB?
You should have your potassium and creatinine checked 1-2 weeks after starting or changing the dose. After that, every 3 months during stable treatment. If you have kidney disease, diabetes, or are over 70, your doctor may check more often. Rising creatinine (more than 30%) or potassium above 5.0 mmol/L means you need a dose adjustment or a different medication.
What’s the best alternative if I need stronger blood pressure control?
Instead of adding another RAS blocker, the safest options are adding a diuretic like hydrochlorothiazide, a calcium channel blocker like amlodipine, or a mineralocorticoid receptor antagonist like spironolactone. For heart failure, sacubitril/valsartan (Entresto) is now preferred over ACE inhibitors alone. SGLT2 inhibitors like dapagliflozin also offer strong kidney and heart protection without the risks of RAS over-blockade.
Are there any new drugs replacing ACE inhibitors and ARBs?
Yes. For heart failure, sacubitril/valsartan (Entresto) has replaced ACE inhibitors as first-line therapy in many cases. For kidney and heart protection in people with diabetes or chronic kidney disease, SGLT2 inhibitors like dapagliflozin and empagliflozin are now recommended alongside or instead of RAS blockers. These newer drugs lower blood pressure, reduce proteinuria, and cut hospitalizations without raising potassium or hurting kidney function the same way.
Tommy Watson
December 13, 2025 AT 05:10so like... u just told me my med is dangerous but didnt say what to do?? like wtf. i’m on lisinopril and my bp is still 150/95. now what?? go buy a treadmill??
Sheldon Bird
December 14, 2025 AT 23:25hey i know this is heavy info but you laid it out so clearly 😊 seriously, this is the kind of post that saves lives. i’ve seen friends get hospitalized from mixing these and no one ever told them it was risky. thanks for the clarity!
Karen Mccullouch
December 15, 2025 AT 20:58THIS IS WHY AMERICA’S HEALTHCARE IS BROKEN. DOCTORS JUST GIVE PILLS LIKE CANDY. I’M NOT SURPRISED PEOPLE ARE DYING FROM STUPID DRUG COMBOS. STOP LETTING PHARMA COMPANIES CONTROL OUR BODIES!!
Shelby Ume
December 17, 2025 AT 11:56Thank you for writing this with such precision and care. The distinction between mechanism of action and clinical outcomes is critical for patient safety. I’ve counseled dozens of patients who were erroneously prescribed dual RAS blockade - and every single one had elevated potassium or renal dysfunction within weeks. The guidelines exist for a reason. Please share this with your provider. It’s not just about blood pressure numbers - it’s about preserving kidney function and preventing arrhythmias.
Jade Hovet
December 17, 2025 AT 22:34omg YES!! 🙌 i switched from lisinopril to losartan cause of the cough and thought i was golden… then my dr checked my K+ and it was 5.6 😳 i had no idea!! now i’m on amlodipine + hctz and feel way better. thank you for this!! 🫶
Himmat Singh
December 19, 2025 AT 02:01While the evidence presented is statistically significant, it is not universally applicable. In certain populations - particularly those with proteinuric nephropathies refractory to monotherapy - dual blockade may offer marginal benefit. The exclusion of such cases from general recommendations constitutes a form of therapeutic oversimplification. Evidence-based medicine must account for heterogeneity.
Jamie Clark
December 20, 2025 AT 19:59They told us this was safe for years. Then they changed the guidelines. Then they made billions off ARNIs and SGLT2 inhibitors. Who benefits? Not the patient. The system just replaced one profitable drug with another. You think this is about health? It’s about market share. Wake up.
Michael Gardner
December 21, 2025 AT 17:20Wait, so if I had angioedema on lisinopril, I can’t take losartan? But what about sacubitril/valsartan? Does that carry the same risk? I’m asking because my doc just switched me to Entresto and I’m nervous.
Willie Onst
December 22, 2025 AT 07:28bro this is why i love reddit. someone actually explains stuff without jargon. i used to think mixing meds was like stacking energy drinks - more = better. now i know it’s more like lighting two candles in a gas leak. don’t do it. 🙏
Ronan Lansbury
December 23, 2025 AT 23:42Did you know the FDA’s 2008 warning on dual RAS blockade was buried under a press release about statin side effects? And that the ONTARGET trial was funded by Boehringer Ingelheim, who makes telmisartan? Coincidence? I think not. The truth is always buried. Always.
nina nakamura
December 25, 2025 AT 10:03